Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 2
Comparison of foetus organ dose and cancer risks in sequential and helical modes in CT pelvimetry for pregnant patients: A Monte Carlo simulation study
Yassine Benameur1,2*, Mohammed Najeh2, Maroine Tahiri1, Mounir Mkimel1, Redouane El Baydaoui1, Bouazza El Hariri1, Mohammed Reda Mesradi1, Abderaouf Hilali1 and Elmadani Saad12Department of radio physics university hospital, Ibn Rochd, Casablanca, Morocco
Yassine Benameur, Hassan First University of Settat, health science and technology laboratory, higher institute of health sciences, Settat, Department of radio physics university hospital, Ibn Rochd, Casablanca,, Morocco, Email: y.benameur@uhp.ac.ma
Received: 05-Feb-2023, Manuscript No. OAR-22-88719 ; Accepted: 23-Feb-2023, Pre QC No. OAR-22-88719 (PQ); Editor assigned: 07-Feb-2023, Pre QC No. OAR-22-88719 (PQ); Reviewed: 15-Feb-2023, QC No. OAR-22-88719 (Q); Revised: 22-Feb-2023, Manuscript No. OAR-22-88719 (R); Published: 25-Feb-2023
Abstract
A pelvic CT scan may be recommended for a pregnant woman in the later stages of pregnancy if there is a possibility that the baby's head may be too large to fit through the pelvis during delivery. This examination assesses the size of the pelvis by measuring different bone diameters and provides information on the pelvis's morphology. Additionally, physicists and doctors frequently worry about ionizing radiation exposure might have a detrimental effect on the foetus. In this study, GATE Monte Carlo toolkit was used to model the SOMATOM EMOTION 16 CT scanner (Siemens Medical Solutions, Erlangen, Germany). The CTDI measurement was used to validate the simulated scanner model for energies 80 kV, 110 kV, and 130 kV. A voxelized phantom in the third trimester was scanned in sequential and helical modes. Organ foetal doses and mean doses were compared at 80 kV, in order to determine the foetal risks associated for each protocol's.
The mean foetal doses for sequential and helical mode are 0.74 mGy and 0.90 mGy, respectively. The risks of childhood cancer were 1 in 16,000 and 1 in 17,000 for sequential and helical modes respectively. The risks of hereditary disease were one in 220,000 and other in 270,000 for sequential and helical modes respectively. Although the cumulative dose to the foetus is thought to be less than 100 mGy, the foetal doses were considered acceptable.
Keywords
pelvic CT, organ dose, voxelized phantom, geant4, gate, pregnant woman, pregnancy voxelized phantom
Introduction
CT scans for pregnant patients may be necessary at times to provide essential clinical information for diagnosis. However, compared to other radiological procedures, this type of examination exposes the patient to a higher dose of radiation. In certain situations, particularly during late pregnancy, pelvimetry may be recommended for the mother when there is a risk that the baby will not pass through the pelvis. This is done by measuring various bone diameters and provides comprehensive information on pelvic morphology. Conventional X-rays, digital fluorography, Computed Tomography (CT) scan, or Magnetic Resonance Imaging (MRI) can all be used to do this purpose [1]. Except MRI pelvimetry, the first three procedures expose mother and foetus to radiation doses that can vary by up to 40 times, depending on how the technique is carried out [2]. The use of Magnetic Resonance Imaging (MRI), a non-irradiating imaging technique that also produces accurate pelvic measurements, is still constrained by availability issues [3].
In practice, CT pelvimetry is the most commonly used method in radiological centres, there are two methods of radiation: The first, sequential mode combines a profile tomogram and two transverse slices passing through the Transverse Median (TM) and Bi-Epineal (BE) diameters [4]. The second method consists of producing fine slices in helical mode and reconstructing these slices in a superposed way to obtain a 3D volume containing all the information independently of the patient's position on the table [5].
It is well-known that irradiation during pregnancy can cause malformations in the developing organ. The threshold for these deterministic effects has been estimated to be 10 cGy [6, 7]. Irradiation of the embryo may also lead to an increased risk of stochastic effects, namely the induction of genetic effects and cancers. Thus, an embryonic dose of less than 10 cGy should not be considered as a reason to terminate a pregnancy. Recognizing the possibility of adverse effects from foetus exposure and the impossibility of direct in vivo measurement, medical physicists have developed several methods to estimate the amount of radiation reaching the foetus. Physicians should understand these methods and how the dose was calculated and related to potential foetus bioeffects.
Several studies have estimated the mean foetus dose using different methods, the study by klarenta et al. study, estimate foetus dose using an anthropomorphic female phantom with gelatine boluses [8]. The uterine wall segmentations representing pregnancy stages were scanned for trauma and abdomino-pelvic using helical mode. Additionally, Matsunaga et al. estimate effective foetus dose in pelvimetry scan using multiple contiguous sections in a 320-row CT and an anthropomorphic [9]. The results were compared with IMPAC CT software.
Another recent study, Mocubangele et al. estimated the mean dose and foetus risk of 194 patients examined by pelvimetry in helical mode [10]. Through the foetal dose web platform using the volumetric Computed Tomography Dose Index (CTDI) obtained from the scanner for each patient.
Today the predominant method for assessment of organ absorbed dose is the use of Monte Carlo (MC) simulations, particularly GATE. Studies that estimate foetus radiation dose using Gate from pelvic CT scans are very limited.
This study consists of three successive steps:
• A measured step to use a PMMA phantom and an ionization chamber to estimate CTDI during a pelvic protocol, then, we compare the experimental results with those obtained by GATE, by modulating the scanner, PMMA phantom and ionization chamber under the same experimental conditions in order to validate the modulated geometry.
• We replace the PMMA phantom with a voxelized phantom of a pregnant patient to estimate foetus organs and means dose during pelvimetry using helical and sequential mode.
• Finally, we estimate the foetus risk for both sequential and helical modes using Fet-Dose software.
Materials and Methods
GATE Monte Carlo platform
A CT scanner is modelled using the Geant4 application for tomographic emission (GATE v8.1), which is a simulator developed in C++ and based on the Geant4 development environment [11]. The basic physics consists in simulating all the physical processes involved in interaction of radiation with matter. T he question of random number generators, which is fundamental in the field of (MC) calculations, is dealt by the CLHEP library, also developed at CERN
Multi detector CT scanner Model
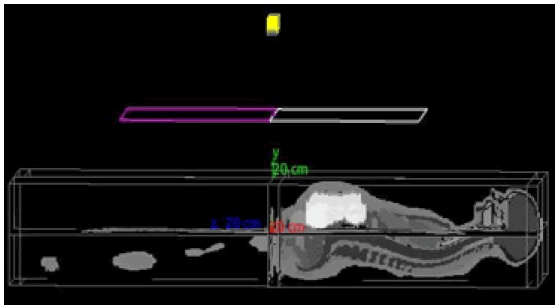
Figure 1, represents a modelled geometry of a CT scanner type Somatom Emotion CT (Siemens Medical. The model includes 16 arrays of detectors added to the CT scanner, with numerous pitch options ranging from 0.5 to 1.5, enabling it to work in both sequential and helical modes. The distances between the iso-centre, focal spot and detector were 536 mm and 941 mm respectively. With two collimators, each with aluminium diameters of 50 cm, 50 cm, and 5 cm for x, y, and z, the fan beam is collimated in the x-y plane at a fan angle of 52°. The X-ray tube's available options are 80kV, 110kV, and 130kV and the current tube ranges from 80 mA to 360 mA.
Figure 1: GATE visualization of CT scan
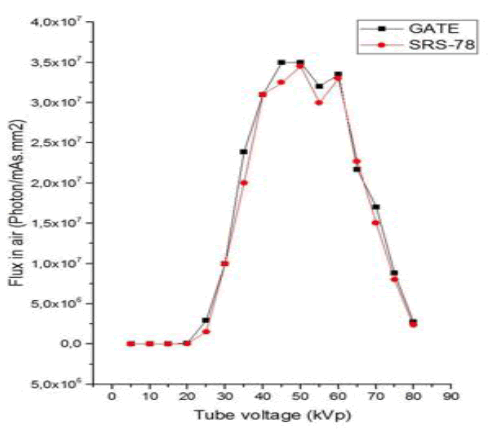
Using the commercial X-ray spectrum generator SRS-78, which was created by the Institute of Physics and Engineering in Medicine, the X-ray spectrum was generated from a Tungsten anode. The created spectrum was added to GATE as a General Particle Source (GPS), which was described as a point source for particles with an isotropic angular distribution provided by the equation (1).
Where φ and θ are the spherical angle coordinates.
In the current study, we employed only the Body Bow-Tie Filter and determined its form's corresponding attenuation. A simplified geometry was used to model the bow-tie filter as rectangles made of aluminium, to calculate the present dose. To improve the Gate MC simulation, we used the commercial X-ray spectrum generator SRS-78 to model the X-ray spectrum emitted from the point source located at the x-ray tube anode (Figure 2).
Figure 2: Normalized X-ray spectrum for a tungsten target at 80 keV was generated using the SRS-78 program and GATE.
KATJA pregnant phantom modelling
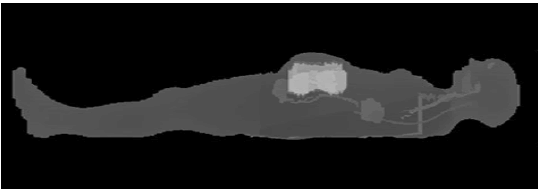
At the Helmholtz Zentrum München German Research Center for Environmental Health, a pregnant woman in her 24th week of pregnancy was previously created as a whole-body vowelized phantom. The "Katja" model combines the ICRP adult female reference phantom and a voxel phantom of a foetus (ICRP 2009a) [12, 13] (Figure 3).
Figure 3: KATJA phantom
A database of abdominal and pelvic regions from a female patient in the 24th week of pregnancy was used to segment the foetus. All organs could be clearly seen and segmented as a The model provided detailed anatomical descriptions of women at approximately six months of pregnancy; the description of the phantom used is shown in Table 1.
Tab. 1. Description of the phantom KATJA
| Feature | KATJA |
|---|---|
| Height | 168.4 cm |
| Weight | 60.3 kg |
| Number of defined organs in patient | 141 |
| Number of defined organs in fetus | 14 |
| Term | 24 |
| Fetus orientation | Head down, spine to left |
| Number of voxels (x, y, z) | (299, 150, 348) |
| Voxel size (x, y, z) | (1.775, 1.775, 4.84) (mm) |
Foetus Dose estimation and risk
Dose by region:
The GATE version (v8.1), allows for the insertion of real clinical data directly into the modelled scanner, such as the voxelized phantom, which enables accurate representation of the real anatomical characteristics of each organ in personalized dosimetry simulations.
The dose actor (dose by region) calculates the total energy deposited, including secondary particles, in each voxel of the phantom. As a result, a 3D dose map in the form of an MHD image file will be generated, where each label defines a region where the energies will be summed, and the dose during the simulation will be calculated. It is important that regions (organs) contain voxels of the same material for accurate dose calculation [11].
Protocols (Mode of scanning simulation):
To compare the dose received by the foetus during two pelvic scanning modes, two simulations were performed using two protocols. The first protocol involves using a simulated scanner in helical mode where the irradiation source (tube) is constantly turn on and rotating around the phantom while the table is moves forward to examine the pelvic region of the phantom. This method allows the doctors to have a 3D reconstruction of the pelvic bone, facilitating the measurements needed for a normal delivery.
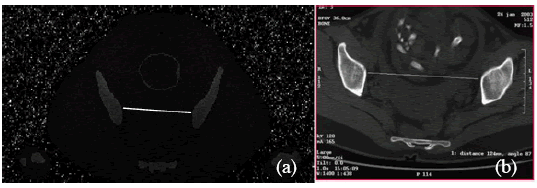
The second protocol (sequential) involves taking two slices only, axial and axial oblique [14]. These slices are sufficient to ensure the foetus passes through the iliac bones, resulting a good delivery (Figure 4b). For this, we used the modelled scanner in sequential mode, where the irradiation source was turned on for the first time to rotate around the phantom without moving the table to take an axial slice perpendicular to the upper strait to measure the median transverse diameter (Figure 4a). The source was turned off and the table moved to the sciatic spine bones of phantom Katja. The source turned on for the second time at an oblique angle to take the second slice (axial oblique) allowing direct measurement of the bi-pineal diameter.
Figure 4: Axial cross-section perpendicular to the upper strait for direct measurement of the median transverse diameter a. simulated b. real slice CT scan
CTDI measurement with PMMA Phantom
A Siemens Somatom Emotion 16-slice scanner is used with a 32cm diameter PMMA phantom to simulate the human body. T he phantom is made of PMMA (ρ=1.19g/cm3), measuring 15 cm in length (Figure 5). The phantom was scanned by the pelvic protocol with the following parameters 80 kV, 100 mAs, pitch=1.
Figure 5: CTDI100 measurement in PMMA body phantom. The phantom has been placed on the CT table with its long axis aligned with the gantry's axis of rotation. It has a diameter of 32 cm.
There is also an ionization chamber (Radcal Corporation 10X63CT) and an electrometer (Radical Corporation USA). The Accu-Gold+ software was used to estimate the absorbed dose. T he system is equipped with a barometer and a thermometer to monitor the experimental conditions in the room.
The dose is assessed by the CT Dose Index (CTDI) which represents the absorbed dose along the Z-axis of the scanner during one rotation of the x-ray source. The CTDI can be measured using a 10cm long pen chamber. The dose is measured in the five positions of the phantom. The weighted dose index CTDIW (mGy) is calculated using the following equations.
Then, we compare the experimental results with those obtained by Gate simulations that model the same materials under the same conditions.
RISK EFFECTS OF FOETUS RADIATION
To estimate the risks of radiation to the foetus after exposure, such as the risk of cancer in the childhood and hereditary effects, the foetus Radiation Risk (R) is calculated using the equation (2) approved by Osei et al. The Fet-Dose program was used to calculate all risk estimations.

Where RC is the Risk Coefficient (Osei, et al., 2003) [15].
Results and Discussion
Table 2 compares the measured and simulated CTDIw, using Equation (5) for all tube voltages of 80, 110, and 130kV. The differences in this study range from 1.32% to 7.21%. It should be noted that the study by Lee et al. also shows a difference of 8.6% between the measured and simulated CTDIw. Variations may be due to differences in simulation conditions, environment, and source [16].
Tab. 2. Measured CTDIw and simulated CTDIw.
| Tube voltage (kVp) | Measured CTDIw (mGy) | Simulated CTDIw (mGy) | Relative difference |
|---|---|---|---|
| 80 | 3.39 ± 0,46 | 3.15 ± 0,38 | 0.07% |
| 110 | 8.27 ± 0,73 | 8.16 ± 0,98 | 0.01% |
| 130 | 12.48 ± 0,93 | 11.78 ± 0,83 | 0.06% |
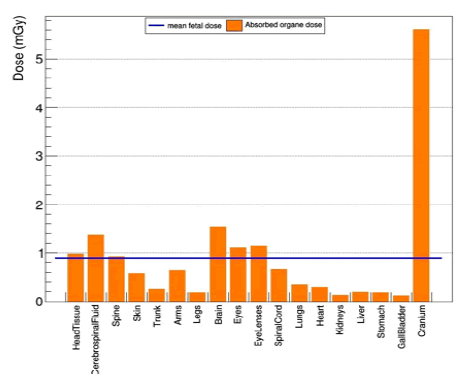
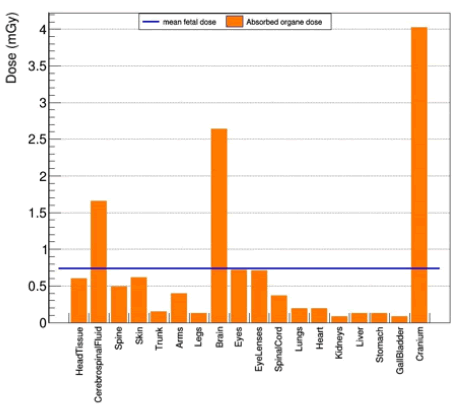
A pelvimetry scan was simulated using the parameters of 80 kV, 100 mAs, and pitch 1 in helical mode, the length of the examination was 26 cm. For all CT acquisitions, the results obtained are analysed to evaluate the impact of using the sequential and helical modes on the dose of radiation received by the foetus’s organs, as shown in Figures 6 and 7.
Figure 6: Organs dose pelvimetry for sequential mode
Figure 7: Organs dose pelvimetry for helical mode
Figures 6 and 7 show the organ dose and mean dose for the helical and sequential modes. It can be observed that the mean foetus dose is reduced by 17.77% between the two methods. In the sequential mode, the dose to all organs is reduced, except for the brain.
All risk estimates were calculated in both sequential and helical modes using Fet-Dose (as presented in Table 3. The estimated risk for childhood cancer associated with an absorbed dose of 0.9 mGy in the helical mode was calculated to be 7.210-5, while 4.5105 was calculated for a hereditary effects and 9.710-5 was served to mental radiation. On the other hand, for an estimated dose of 0.74 mGy in sequential mode, we found that the risk of developing childhood cancer due to the absorbed dose was 5.910-5. The risk for hereditary effects was calculated to be 3.710-5, and the risk for mental radiation was calculated to be 7.710-5.
Tab. 3. Mean foetal dose and risk of childhood cancers, hereditary effects and serve mental radiation for helical and sequential mode.
| Mode scanning | Fetus dose (mGy) | Childhood cancer | Hereditary effects | Serve mental radiation |
|---|---|---|---|---|
| Helical | 0.9 | 7.210-5 | 4.5 10-5 | 9.710-5 |
| Sequential | 0.74 | 5.910-5 | 3.7 10-5 | 7.710-5 |
Following previous studies, The Baseline Model (BM) estimated 360,114 total childhood cancers occurring worldwide in 2015; 54% in Asia and 28% in Africa. BM estimated standardized rates ranged from ~178 cases per million in Europe and North America, to ~218 cases per million in West and Middle Africa [17].
The probability of having a radio-inducted late cancer due to the stochastic effect of absorbed radiation in the foetus in this study was estimated to be 1 in 14.000, table 4 shows in detail the major effect calculated, the risks generally are very low compared to natural incidence and genetic disorders. Thus the increase of genetic impact for risks is negligible compared to natural risk of genetic disease.
Tab. 4. Mean fetal dose and risk of childhood cancers, hereditary effects and serve mental radiation for helical and sequential mode
| Mode scanning | Childhood cancer | Hereditary effects | Serve mental radiation |
|---|---|---|---|
| Helical | 1 in 14.000 | 1 in 220.000 | 1 in 10.000 |
| Sequential | 1 in 17.000 | 1 in 270.000 | 1 in 13.000 |
The stochastic effects of radiation are incredible in most cases and the evaluation of these risks is generally probabilistic due the small effect on the genetic composition of the foetus and growth after birth.
Since the foetus dose in the sequential mode has not been reported in the literature, we only compared the foetus dose received by the helical mode.
In order to compare the mean foetus dose in this study to other studies found in the literature, our results show good agreement with those of Phexell et al. [18] which gave a mean foetus dose of 0.8 mGy using an anthropomorphic female phantom and bags filled with sodium chloride to simulate the last month of pregnancy.
Otherwise, the highest difference observed is that of Matsunga et al. [9] utilizing RPI computational phantoms and Impact CT simulations. Slimane et al. [19] reported a mean foetus dose of 2.36 mGy, which was obtained by of examining a total of 30 patients using SIEMENS Somatom Sensation 64 CT set at 110 kV and 30 mA. Our value is lower than that reported by Mokubangele et al. (1.5 mGy), who used a statistical study for 130 patients examined. Results reveal that overall doses received by foetus organs were less than 100 mGy.
These observed differences were likely caused by uncertainties in the X-ray spectrum (filtration), kV, pitch, mAs, modelled geometry, phantom volume, foetus age and organ density.
The risk for the foetus to develop a radio-induced cancer in childhood is a possible outcome after pregnant women undergo radiation exposure. Examination and investigation after delivery is clinically necessity. Or these examinations using spiral methods for pregnant women should be clinically justified and dose is kept to a minimum while still consistent with the diagnostic requirements.
Conclusion
The radiation exposure during sequential and helical CT- pelvimetry exams is minimal, with a low risk of causing childhood cancers or hereditary diseases. As the radiation absorbed by the foetus during CT scans is minimal, it's worth considering further use of the technology to improve diagnostic accuracy.
References
- Sibony O, Alran S, Oury JF. Vaginal birth after cesarean section: X-ray pelvimetry at term is informative.
- Thomas SM, Bees NR, Adam EJ. Trends in the use of pelvimetry techniques. Clinical radiology. 1998;53:293-295.
- Aubry S, Padoin P, Petegnief Y, Vidal C, Riethmuller D, Delabrousse E. Can three-dimensional pelvimetry using low-dose stereoradiography replace low-dose CT pelvimetry? Diagn Interv Imaging. 2018; 99:569-576.
- Camus M, Buthiau D, Vauthier D, Heitz F, Darbois Y. Pelvimétrie par tomodensitométrie. J Gynécol Obstét Biol Reprod. 1987; 16:327-333.
- Balleyguier C, Jouanic JM, Corréas JM, Benachi A, Dumez Y, et al. La pelvimétrie volumique en scanographie hélicoïdale multibarrettes. J Radiol. 2003; 84:425-427.
- Doshi SK, Negus IS, Oduko JM. Foetusradiation dose from CT pulmonary angiography in late pregnancy: a phantom study. Br J Radiol. 2008; 81:653-658.
- Victoria T, Epelman M, Coleman BG, Horii S, Oliver ER, et al. Low-dose foetusCT in the prenatal evaluation of skeletal dysplasias and other severe skeletal abnormalities. Am J Roentgenol. 2013; 200:989-1000.
- Kelaranta A, Makela T, Kaasalainen T, Kortesniemi M. Foetusradiation dose in three common CT examinations during pregnancy–Monte Carlo study. Physica Medica. 2017; 43:199-206.
- Matsunaga Y, Kawaguchi A, Kobayashi M, Suzuki S, Suzuki S, et al. Dose evaluation for foetal computed tomography with a 320-row unit in wide-volume mode and an 80-row unit in helical scanning mode: a phantom study. Radiat Prot Dosim. 2016; 168:523-30.
- Mokubangele CM, Ebongue AN, Bongue D, Ndontchueng MM, Moifo B. Evaluation of the Fetal-Maternal Radiation Doses in CT-Pelvimetry and Estimation of the FoetusRadiation Risks in 03 Radiology Departments in Douala-Cameroon. Open J Radiol. 2022; 12:113-124.
- Tahiri M, Mkimel M, Benameur Y, El Baydaoui R, Mesradi MR, El Rhazouani O. Organ Dose Estimation for Adult Chest CT Examination Using GATE Monte Carlo Simulation. Phys Part Nucl Lett. 2021;18:502-509.
- Becker J, Zankl M, Fill U, Hoeschen C. Katja-The 24th week of virtual pregnancy for dosimetric calculations. Pol J Med Phys Eng. 2008;14:13.
- Protection R. ICRP publication 103. Ann ICRP. 2007;37:2.
- Buthiau D. La pelvimétrie par scanner: état des connaissances actuelles: Obstétrique. Lett. du gynécol. 2002:19-25.
- Osei EK, Darko JB, Faulkner K, Kotre CJ. Software for the estimation of foetal radiation dose to patients and staff in diagnostic radiology. J. Radiol. Prot. 2003; 23:183.
- Lee C, Lodwick D, Hurtado J, Pafundi D, Williams JL, Bolch WE. The UF family of reference hybrid phantoms for computational radiation dosimetry. Phys Med Biol. 2009; 55:339.
- Osei EK, Darko J. Foetal radiation dose and risk from diagnostic radiology procedures: a multinational study. Int Sch Res Not. 2013;2013.
- Phexell E, Soderberg M, Bolejko A. Estimation of foetal radiation dose in a comparative study of pelvimetry with conventional radiography and different computer tomography methods. Int J Radiol Radiat Ther. 2018; 5:243-247.
- Semghouli S, Amaoui B, Hakam OK, Choukri A. Radiation exposure during pelvimetry CT procedures in Ibn Sina Children's Hospital of Rabat. Radiat Phys Chem 2020; 175:108087.