Case Report - Onkologia i Radioterapia ( 2022) Volume 16, Issue 9
Unusual mediastinal paraganglioma with single pulmonary metastasis: A case report
Hassani W1, Alaoui chrifi G1, Farhane F1, Alami Z1, Alami B2 and Bouhafa T12Radiology department, University Hospital Centre, Hassan II, Fes, Morocco
Received: 29-Aug-2022, Manuscript No. OAR-22-73172; Accepted: 21-Sep-2022, Pre QC No. OAR-22-73172 (PQ); Editor assigned: 31-Aug-2022, Pre QC No. OAR-22-73172 (PQ); Reviewed: 16-Sep-2022, QC No. OAR-22-73172 (Q); Revised: 19-Sep-2022, Manuscript No. OAR-22-73172 (R); Published: 22-Sep-2022
Abstract
Background: Malignant paragangliomas are a real challenge for practitioners. They are rare complex tumours, very heterogeneous in their evolution and prognosis. Given the rarity of this group of tumours, there is no consensus on therapeutic management. surgical resection is considered the treatment of choice.
Case Description: We report a very rare case of a 73-year-old patient presenting a malignant non-functional mediastinal paraganglioma with a single pulmonary metastasis deemed unrespectable and treated with radiation therapy.
Conclusions: This study aims to highlight the use of radiotherapy as an interesting therapeutic option in the management of malignant mediastinal paragangliomas not suitable for surgery.
Keywords
mediastinal paraganglioma, case report, radiotherapy
Introduction
Mediastinal paragangliomas are rare tumours. They can have a neuroendocrine activity or be non-functional, incidental, often asymptomatic, or cause mass effect symptoms.
they are of difficult diagnosis and should be considered malignant tumours, due to the potential aggressive behaviour of cases with high mitotic index and the frequent possibility of recurrence and metastases
Although low-grade tumours, they can display aggressive behaviour, developing local infiltration and distant metastases.
Surgical resection is considered the treatment of choice and careful intraoperative manipulation is recommended, due to the high vascularity of these tumours, to prevent complications. However, in some cases, surgery can be difficult due to particular or multiple tumour sites and may cause severe neurological deficits. In such cases, radiotherapy can be an effective alternative.
We report here a very rare case of an endothoracic mediastinal paraganglioma and suggest a literature review of this rare entity
Case Presentation
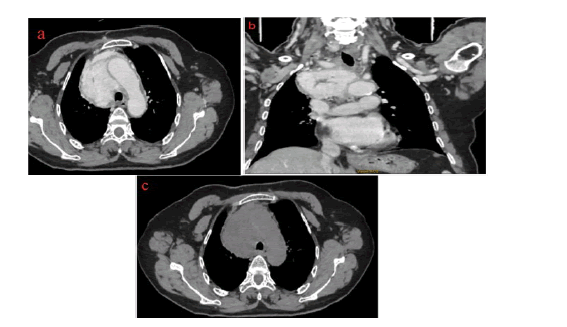
A 62-year-old female patient with no medical history was admitted for the management of thoracic trauma caused by a road traffic injury. The mediastinal paraganglioma was incidentally discovered after a thoracic imaging CT (Figure 1).
Figure 1:Chest CT showing an anterior mediastinal lesion, with well-defined contours, heterogeneously enhanced after contrast containing some areas of necrosis
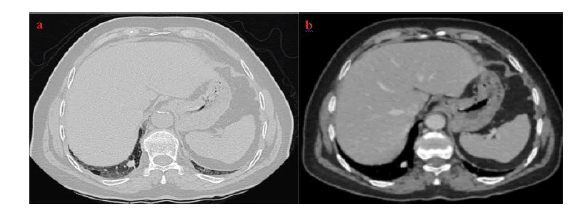
It was associated with a single lung metastasis discovered in the same CT scan presenting the same characteristics (Figure 2).
Figure 2: Chest CT scan showing a pulmonary nodule on the right lower lobe, secondary appearance
Hence her consultation, she runs through a mediastinoscopy and a biopsy that found a paraganglioma in the pathology
The paraganglioma was non-functional:
Normetanephrine: at 0.28 µmol/24h (0.07-0.38), Metanephrine at 0.68 µmol/24h (0.20-1), 3 OMD at 0.73 µmol/24h (0.50- 1.6) and Chromogranin A at 93 ng/ml (<102).
The case was discussed in a multidisciplinary consultation meeting and the malignant, non-functional paraganglioma was deemed unrespectable and the decision was to use radiotherapy for treatment.
A 123I-mIBG Scintigraphy was also performed, showing a frank uptake of MIBG next to the anterior mediastinal tumour mass in favour of paraganglioma and an absence of any other source of pathological uptake at a distance.
The mediastinal tumour was treated with three-dimensional (3D) conformal radiation therapy using 18 MeV photons. 50 grey were administrated in the target volume with a daily fraction of 2 greys. The therapy was well tolerated.
The treatment was initiated in February and completed in March 2022.
Discussion
Paragangliomas of the mediastinum are rare, approximately 150 cases only were reported in the literature [1], accounting for less than 0.3% of mediastinal masses, more commonly occurring in the posterior mediastinum. these tumours are slow growing and rarely malignant. They can arise from either parasympathetic or sympathetic paraganglia; two types occur with similar frequency [2,3]. Parasympathetic ganglia-derived paragangliomas are mainly located in the head and skull base along the branches of the glossopharyngeal and vagus nerves. Sympathetic ganglia-derived paragangliomas arise outside of the adrenal gland anywhere along the sympathetic chain, with the majority occurring in the abdomen (75%) [3]. These tumours arise from the paravertebral aortosympathetic paraganglia in the posterior or from the aortopulmonary paraganglia in the middle mediastinum.
Most paragangliomas do not produce symptoms, however, they can secrete catecholamines leading to symptoms such as sweating, headaches, tachycardia, and hypertension. The majority are asymptomatic and non–catecholamine-secreting tumours, but they can produce chest discomfort or neurological symptoms. These tumours can be identified in imaging studies, often located at the bifurcation of the great vessels [3]. Differential diagnosis includes lymphadenopathy, duplication cyst, pericardial cyst, tracheal lesion, aortic arch aneurysm, or enlarged pulmonary artery.
Mediastinal paragangliomas may develop particularly aggressive behaviour and are associated with higher morbidity and mortality [4-6], with distant metastasis rates reported as 19.5% and 26.6% in two review studies [7, 8]. The diagnosis of malignancy cannot be made reliably from the histologic appearance of the tumour and is based on the presence of metastases to the regional lymph nodes or distant sites, such as the lungs or bone [9]. Therefore, in limited disease and whenever possible, complete surgical resection should always be the treatment of choice. In almost 25 years of experience at the Mayo Clinic on 14 mediastinal paraganglioma patients, a complete resection rate of 76.9% and a mortality rate of 7.1% were reported [4].
We believe that in patients affected by unrespectable paragangliomas radiotherapy is a safe and effective alternative to surgery. The use of high-dose conformity techniques such as 3D-CRT and IMRT will allow higher local control rates with relatively few side effects thanks to the possibility of dose escalation and reduction of the amount of irradiated healthy tissues
Valdagni and AmichettP reported seven patients (13 lesions) treated with radiotherapy for carotid body paragangliomas between 1968 and 1987. Treatment consisted of radiotherapy as the sole treatment modality (10 lesions) or after surgery (3 lesions). Follow-ups ranged from 1 year to 19 years; the median follow-up interval was not stated. Total doses ranged from 46 Gy to 60 Gy at 1.8 Gy to 2.5 Gy per fraction. Local control was achieved in all patients. Acute side effects were minimal; no short- or longterm toxicities were noted [10].
Prognosis in malignant paragangliomas is impacted by tumour burden, location of metastases, and rate of progression. In one review of patients with metastatic paraganglioma, the overall and disease-specific survivals were 24.6 years and 33.7 years, respectively [1]. In one series of 192 patients, the five-year probability of recurrence was 20% in secretory extra-adrenal paraganglioma [10]. Given the risk of local recurrence and metastases, lifelong surveillance with imaging or biochemical testing in cases of secretory paraganglioma is warranted.
Conclusion
Paragangliomas are rare neuroendocrine tumours that can be difficult to manage. Novel radiotherapy techniques can be an interesting option for an inoperable patient. Further prospective studies may suggest optimal dose and fractionation.
References
- Takashima Y, Kamitani T, Kawanami S, Nagao M, Yonezawa M, et al. Mediastinal paraganglioma. Jpn J Radiol Juill. 2015; 33:433â??436.
- Buchanan SN, Radecki KM, Chambers LW. Mediastinal paraganglioma. Ann Thorac Surg. 2017;103:e413-414.
- Paul S, Jain SH, Gallegos RP, Aranki SF, Bueno R. Functional paraganglioma of the middle mediastinum. Ann Thorac Surg. 2007;83:e14-16.
- Brown ML, Zayas GE, Abel MD, Young Jr WF, Schaff HV. Mediastinal paragangliomas: the mayo clinic experience. Ann Thorac Surg. 2008; 86:946-951.
- Wald O, Shapira OM, Murar A, Izhar U. Paraganglioma of the mediastinum: challenges in diagnosis and surgical management. J Cardiothorac Surg. 2010;5:1-3.
- Rahi MS, Gunasekaran K, Amoah K, Rudolph D. Paraganglioma of the middle mediastinum. Respir Med Case Rep. 2020; 31:101211.
- Lin MW, Chang YL, Lee YC, Huang PM. Non-functional paraganglioma of the posterior mediastinum. Interact. CardioVasc Thorac Surg.2009; 9:540-542.
- Afani L, Errihani H, Awada A. Therapeutic management of malignant paragangliomas: literature review through an illustrative case. Pan Afr Med J. 2019;32.
- Olson JL, Salyer MW. Mediastinal paragangliomas (aortic body tumor). A report of four cases and a review of the literature. Cancer. 1978;41:2405-2412.
- Nwose P, Galbis JM, Okafor O, Torre W. Mediastinal paraganglioma: A case report. Thorac Cardiovasc Surg.1998; 46:376â??379.