Research - Onkologia i Radioterapia ( 2023) Volume 17, Issue 9
The effect of target volumes on the essential treatment plan parameter and prescription dose for the patients with vestibular schwannoma
Nadiya Y Mohammed*Nadiya Y Mohammed, Department Physiology, College of Medicine, Baghdad University, Baghdad, Iraq, Email: nadiyaym@comed.uobaghdad.edu.iq
Received: 27-Jul-2023, Manuscript No. OAR-23-108227; Accepted: 15-Sep-2023, Pre QC No. OAR-23-108227 (PQ); Editor assigned: 29-Jul-2023, Pre QC No. OAR-23-108227 (PQ); Reviewed: 15-Aug-2023, QC No. OAR-23-108227 (Q); Revised: 25-Aug-2023, Manuscript No. OAR-23-108227 (R); Published: 20-Sep-2023
Abstract
Background: Gamma Knife Radiosurgery (GKRS) is confirmed lately to have a feasible tumor dominance and is much more probable to exclude the cranial neuropathies as the result of open surgery. This study is aimed to investigate the effect of the target volume on the assessment of the essential plan parameters including (Conformality index, Selectivity, Coverage, and Gradient Index (GIn), which are followed in (GKRS) treatment for patients with vestibular schwannoma. Methods: The Target Volume (TV) was identified for each treatment plan and involved 50 patients who underwent Stereotactic Radiosurgery (SRS) treatment for vestibular schwannoma. The assessment parameters were determined to calculate: Coverage (Cov), Selectivity (Slec), Gradient Index (GI), and Paddick Conformance Index (PCI). Result: In this study, the volumes were separated into two groups: group 1 had an average size of 2.20 ± 1.28, while Group 2 had an average size of 9.17 ± 3.95. The mean values of measurements in the two groups were as follows: Cov=0.94 and 0.93, Slec=0.69 and 0.78, GI=2.8 and 2.55, PCI=0.65 and 0.73, and time =19.6 seconds and 34.4 seconds. The dosage distribution was the same for both treatment and reference programs. Conclusion: This study demonstrated that the target volume can affect the essential plan parameters specifically during the evaluation of dose distribution in a treatment plan for vestibular showanoma.
Keywords
target Volume (TV), Coverage (Cov), Selectivity (Slec), Gradient Index (GI), Paddick Conformity Index (PCI)
Introduction
The LGK is a non-invasive radiosurgery equipment that is used to treat brain tumors, AVMs, and other neurological problems. Lars Leksell, a Swedish neurosurgeon, invented it and initially used it in the 1960s [1].
The Gamma Knife is different from traditional surgery in that it uses precise beams of gamma radiation oriented to the target and treated specific areas in the brain instead of incisions or invasive procedures. The treatment is carried out in a single session, and the radiation beams converge at the target location, delivering a high dose of radiation with minimizing exposure to surrounding healthy tissue [2]. It's interesting to consider that the Gamma Knife is a powerful tool for certain brain conditions, and it may be considered not suitable for all patients or conditions [3].
The treatment planning process creates a detailed threedimensional map of the tumor and surrounding structures [4]. This allows the medical team to calculate the appropriate radiation dose and develop a therapeutic strategy that provides a high dose of radiation to the tumor while little to surrounding sensitive areas including the brainstem and cranial nerves [5, 6].
During the procedure, the patient's head is immobilized using a headframe or a custom-made mask, to ensure accurate targeting. Before treatment, imaging tests such as MRI or CT scans are performed to precisely locate and map the tumor's position and size [7, 8].
For vestibular schwannomas (also known as auditory neuromas), stereotactic radiation, including the use of the Gamma Knife, can be a viable therapeutic option [6].
GKRS is a well-established treatment option for vestibular schwannomas, especially for targets who may not be removed by surgery due to various factors such as tumor size, patient age, or overall health [9].
The decision should be determined by the neurosurgeon in considering the GKRS as a treatment procedure taking into account the clinical situation, the mass effect, and tumor size. Mostly, the tumor size which is less than 3 cm were treated with GKRS [10, 11].
Regardless of the obtained data from GKRS treatment regarding the radiographic clinical parameters, there was no evidence study to ensure the correlation between the target volume and the essential treatment plan parameters. This study is established to indicate, the relation between target volumes of VSs and their effect on the assessment plan indexes including Conformality index, Selectivity, Coverage, and Gradient index (GIn), (which are followed in (GKRS) treatment for patients with vestibular showanoma)[12, 13].
Materials and Methods
The study was conducted over six months at both the Dr. Saad Al-Witry Hospital for Neurosciences (from September 2022 to January 2023). This study included 50 patients diagnosed with VSs by an oncologist or a neurosurgeon. All patients underwent GKRS treatment at Dr. Saad Alwitry Neuroscience Hospital.
Exclusion criteria included
• Pregnant patients
• Patients with very large diameters great than 3 cm meningiomas.
Stereotactic radiosurgery
The LGK icon system was used to treat the patients. The Evaluation plan metrics included in the study were as follows prescription dose, Covarge (cov), selectivity (slec), Gradient Index (GI), Paddick Conformity Index (PCI), and beam on time.
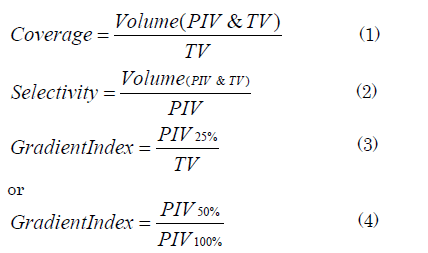
Volumes and doses were known with the use of Dose-Volume Histograms (DVH). The following were used to calculate the Covslec, GI, and PCI [14].

Dosing to organ at risk
The Organs-At-Risk (ORS) included the brainstem and/or the optic nerve, depending on the location of the vestibular schwannoma. The whole essential anatomy was contoured for tumors around the optic nerve. The brainstem was contoured 1 cm cranial to and 1 cm caudal to the tumor level for malignancies near the brainstem. Among the dosimetric measurements recorded were the maximum dose to the optic nerve, the volume of the optic nerve receiving 8 Gy, the maximum dose to the Brain Stem (BSMD), and the volume of the brainstem receiving 12 Gy [15, 16].
Statistical methods
The study employed univariate logistic regression analysis. To study the connection between base plan parameter data and various CVA target volumes. The target volumes in the study were separated into two groups in the analysis, the first with sizes less than 4 cm and the second with sizes larger than 4 cm. The critical plan parameters were determined for each group and compared to the tumor's goal volume.
Result and Discussion
During the scientific investigation period, 50 patients with vestibular schwannoma were treated with GKRS. Tables 1 and 2 indicate patient and therapy characteristics, respectively. The median age at the time of therapy was 47 years ± 8.7 years.
Tab 1. Patient characteristics
| Data | Number of patients | Mean ±SD | Max | Min | |
|---|---|---|---|---|---|
| Age | 50 | 47±8.7 | 13 | 66 | |
| Target volume | Group1>4cm3 | 25 | 2.20±1.28 | 3.911 | 0.079 |
| Group2<4cm3 | 25 | 9.17±3.95 | 20.97 | 4.11 | |
Tab 2. Tumor and treatment characteristics
| Parameter | Group 1 | Group2 | p-value |
|---|---|---|---|
| Selectivity | 0.69 | 0.78 | 0.0430* |
| Covarage | 0.94 | 0.93 | 0.4961* |
| Gradint index | 2.8 | 2.55 | 0.0480* |
| Time | 19.66 | 34.41 | 0.0000* |
| Paddick conformity index | 0.65 | 0.73 | 0.0553 |
The results revealed the statistical analysis of different parameters between Group 1 and Group 2. The p-values indicate whether there is a statistically significant difference between the two groups for each parameter:
• Selectivity: The parameter showed a significant difference between Group 1 and Group 2, with a p-value of 0.0430. • Coverage: The p-value is recorded as 0.4961, this implied that there was no statistically significant difference between Groups 1 and 2.
• Gradient index: The p-value was recorded as 0.0480. This indicated a significant difference between Group 1 and Group 2.
• Time: The p-value was predicted a value of 0.0, which was shown a highly significant difference between Group 1 and Group 2.
• Paddick Conformity Index (PCI): The p-value yielded 0.0553. This was implified that there was no significant difference between Group 1 and Group 2, although the difference is close to being statistically significant.
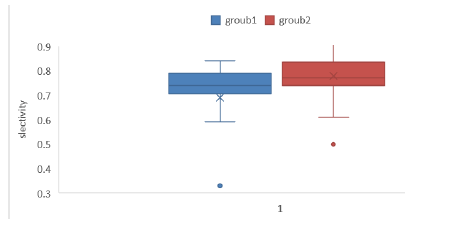
Selectivity (Slec), defined as the proportion of Prescribed Isodose Volume (PIV) inside (TV), can be determined using the inverse of the conformance index multiplied by coverage or given by the program Gamma Plan. The lower and higher selectivity values were 0.20 and 0.84, respectively, found in the group 1 plan assessed in this study, while groub2 were recorded between 0.50 and 0.91. Taking this range into account, Figure 1 shows the selectivity (Slec) index as a function of the target volume.
Figure 1: Different in selectivity between two groups
Selectivity (S)
The acquired results in Figure 1 were compared between the two groups. When the goal volume value increased, the selectivity value increased as well. Some plans had very poor selectivity, and when these plans are evaluated, it is discovered that these low values are attributable to isodose prescriptions that are less than 50%
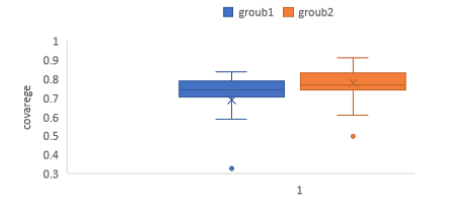
Gamma Plan coverage (Cov) is smaller and bigger coverage values for group 1 plans tested in this study were 0.73 and 0.99, while for group 2 they were 0.86 and 0.99. With this range in mind, Figure 2 displays the coverage (Cov) as a function of the target volume.
Figure 2: Different coverage between two groups
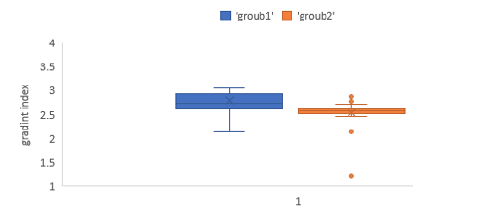
The Gradient Index (GI) was defined as the volume encompassed by half of the prescribed dosage divided by the volume covered by the doctor's suggested dose. For all designs examined in this study, the gradient index values for group 1 and group 2 were 2.49 & 4.3 respectively. Figure 3 represents the gradient index (GI) differential for two groups of the target volume within this range.
Gradient Index (GI)
The information received was in Figure 3, the findings were compared between two groups. It is clear that the bigger the target volume value, the less than or equal to 3 the value of the Gradient Index, which is used to measure the quality of a radiosurgery plan using gamma Knife® equipment. It is also clear that on a plane, the gradient index has a large value. When this technique is tested, it is revealed that greater GI values are connected with prescription doses that are less than 50% of the isodose center.
Figure 3: Different in GI between two groups
Our findings confirm those of Donya and his team, who found that GI and selectivity were essential in making predictions, followed by the Paddick conformity index [17]
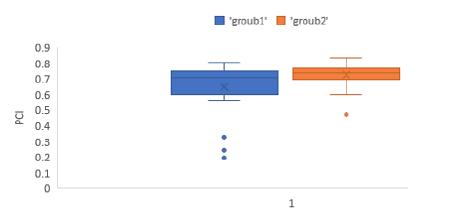
Paddick Conformity Index (PCI): As with the selectivity study, certain plans had a very low conformity index, and examining these plans revealed that these low values were attributable to isodose prescriptions that are less than 50% of the isodose center (Figure 4).
Figure 4: Different in Paddick conformity index between two groups
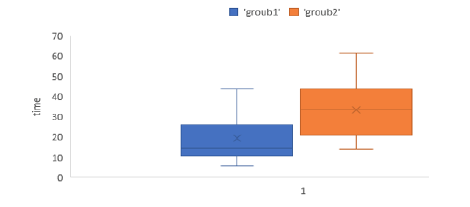
The values obtained by considering the beam on time are displayed in Figure 5. It was clear that the value of the beam on time grew dramatically with group 2 (as the goal volume increased), where the treatment time increased as the goal volume increased. The findings of this study on CVA volume were consistent with those of Lomax and his colleagues who reported that for target volumes of 1 cm3 , a small increase in the volume treated to the prescribed dosage (even by 1 mm) is associated with a statistically significant increase in the total amount treated.
Figure 5: Different of the beam on time between two groups
Conclusion
A large volume generally outperforms a small target volume in terms of selectivity, while a small volume has a higher gradient index. Additionally, a large volume takes longer to achieve the measured parameter compared to a small volume. The coverage and Paddick conformity index do not exhibit significant differences between the two groups, although the latter is marginally close to significance
References
- Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA (2016) 316:401–9.
- Hamza Fares, B., Abdulhussain-Al-Tememy, H., Abbas Abdulmajeed, B., Molecular Study of INF gamma Gene in Aborted Placenta Induced by Brucella Melitensis in Ewes, J Phys.: Conf Ser, 2019.
- Hade, N.A., Ramadhan, R.S., Faraj, M.K. Genetic Polymorphism in Braf Gene Associated with The Incidence of Brain Tumors in a Sample of Iraqi Patients, Biochemical and Cellular Archives, 2020.
[Google Scholar] [Crossref]
- EJ Lehrer, HM McGee, JL Peterson, et al. Stereotactic radiosurgery and immune checkpoint inhibitors in the management of brain metastases. J Mol Sci, 19 (2018), 1-18.
- Arvold ND, Lee EQ, Mehta MP, Margolin K, Alexander BM, Lin NU. Updates in the management of brain metastases. Neuro Oncol. (2016) 18:1043–65. [Google Scholar] [Crossref]
- Minniti G, Scaringi C, Paolini S, Lanzetta G, Romano A, Cicone F. Single-fraction versus multifraction (3 x 9 Gy) stereotactic radiosurgery for large (>2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys. (2016) 95:1142–8. [Google Scholar] [Crossref]
- F Muller-Riemenschneider, A Bockelbrink, I Ernst, et al. Stereotactic radiosurgery for the treatment of brain metastases. Radiotherapy Oncol, 91 (2009), pp. 67-74. [Google Scholar] [Crossref]
- B Lippitz, C Lindquist, I Paddick, D Peterson, K O'Neill, R Beaney. Stereotactic radiosurgery in the treatment of brain metastases. Cancer Treat Rev, 40 (2014);48-59. [Google Scholar] [Crossref]
- Victor X Fu , Jeroen B Verheul , Guus N Beute. Retreatment of vestibular schwannoma with Gamma Knife radiosurgery, clinical outcome, tumor control, and review of literature. J Neurosurg, 2018. [Google Scholar] [Crossref]
- Moneer K. Faraj MD, The efficiency of the prescribed dose of the gamma knife for the treatment of trigeminal neuralgia. Interdisciplinary Neurosurgery, 2018, 9-13. [Google Scholar] [Crossref]
- Bassam Mahmood Flamerz Arkawazi 1, Moneer K Faraj 2, Zaid Al-Attar. Short Term Effectiveness of Gamma Knife Radiosurgery in the Management of Brain Arteriovenous Malformation; Open Access Maced J Med Sci. 2019; 7: 3221-3224. [Google Scholar] [Crossref]
- Tae Won Yoo, M.D., Eun Suk Park, M.D., Do Hoon Kwon. Gamma Knife Radiosurgery for Brainstem Metastasis. J Korean Neurosurg Soc. 2011; 50: 299–303. [Google Scholar] [Crossref]
- Crystian W, Chagas S, Simone CC, Daniela PG. Gamma Knife radiosurgery for vestibular schwannomas: Evaluation of planning using the sphericity degree of the target volume. PLoS One. 2020; 15: e0225638. [Google Scholar] [Crossref]
- Donya, H., Othman, S. and Dimitriadis, A. Evaluating and predicting the Efficiency Index for Stereotactic Radiosurgery Plans using RapidMiner GO(JAVA) Based Artificial Intelligence Algorithms. 2022. [Google Scholar] [Crossref]
- Lomax, N.J. and Scheib, S.G. Quantifying the degree of conformity in radiosurgery treatment planning. Int. J. Radiat. Oncol. Biol. Phys., 2003, 55. [Google Scholar] [Crossref]
- Prabhuraj A.R., Ujwal Y, Arivazhagan A, Narasinga Rao K.V.L., Dhananjaya I. B et al. Effect of Gamma Knife Radiosurgery on Vestibular Schwannoma with Serviceable Hearing: A Single-Center Indian Study. World Neurosurg., 2019; 127: e114-e123. [Google Scholar] [Crossref]
- Yeole U, Prabhuraj A. R., Arivazhagan A, Vazhayil NV. Gamma Knife Radiosurgery for Large Vestibular Schwannoma More Than 10 cm3: A Single-Center Indian Study. J Neurol Surg B Skull Base.2022; 83: e343–e352. [Google Scholar] [Crossref]