Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 5
Testicular Embryonal Carcinoma in the patient with undescended testicle
Nuraj Petrit* and Oruqi MusaNuraj Petrit, Department of Urology, University Clinical Center of Kosovo, Prishtina, Republic of Kosovo, Email: petrit.nuraj@uni-pr.edu
Received: 03-May-2023, Manuscript No. OAR-23-97579; Accepted: 28-May-2023, Pre QC No. OAR-23-97579 (PQ); Editor assigned: 09-May-2023, Pre QC No. OAR-23-97579 (PQ); Reviewed: 19-May-2023, QC No. OAR-23-97579 (Q); Revised: 26-May-2023, Manuscript No. OAR-23-97579 (R); Published: 29-May-2023
Abstract
One 43-year-old male presents in Emergency with left inguinal pain and a mass in the inguinal region. The abdominal surgeon was consulted, who notices a palpation and hard formation in the left inguinal region, which was grown, what raised the suspicion of an incarcerated inguinal hernia. The abdominal surgeon lists the patient for immediate surgical intervention, accessing through the inguinal region. Going through the layers, the formation was reached, which was when it was realized that we are dealing with an undescended testicle tumour. The urologist was called to the surgery room, which then discovers that we are dealing with a tumour of undescended testicle. Left inguinal radical orchiectomy and mass biopsy were performed. Histopathological diagnosis revealed Embryonal carcinoma. Computed tomographic (CT) scan showed multiple metastases: retroperitoneal lymph nodes, and lungs and liver metastasis. Tumour markers elevated; Beta HCG: 1432 mIU/mL, AFP: 409 ng/ml, LDH: 1007 U/L. Chemotherapy was started three weeks after the surgery, with the Bleomycin, Etoposide, and Cisplatin (BEP) regimen, and this cycle was repeated three times, every three weeks, up to three times. After Chemotherapy the tumour markers results were as following: HCG: 4, AFP: 4.8, LDH: 450 U/L. After 3 months CT scan showed, the lungs and liver metastasis seem to have disappeared, and the retroperitoneal lymph nodes were decreased in size. After chemotherapy, retroperitoneal lymph nodes dissection was performed. Microscopic examination revealed no viable cancer cells. After retroperitoneal lymph nodes dissection, the tumour markers results were as following: HCG: 1.0, AFP: 3.6, LDH: 156 U/L. On CT scan, no retroperitoneal, liver, or lungs tumour was detected.
https://marmaris.tours
https://getmarmaristour.com
https://dailytourmarmaris.com
https://marmaristourguide.com
https://marmaris.live
https://marmaris.world
https://marmaris.yachts
Keywords
embryonal carcinoma, undescended testicle, chemotherapy, metastasis.
Introduction
Testicular cancer is relatively rare, accounting for approximately 1%-1.5% of all cancers in men.
Embryonal carcinoma is a type of testicular cancer and part of a group of cancers known as Germ-Cell Tumours (GCT). There are two main types of GCT: Non-Seminomatous Germ Cell Tumors (NSGCT) and seminoma. Non-Seminomatous Germ Cell Tumours (NSGCT) are: embryonal carcinoma, Yolk Sac Tumour (YST), choriocarcinoma, and teratoma [1].
Embryonal carcinoma is an aggressive type of germ-cell tumour that frequently spreads to other parts of the body. Embryonal carcinoma can secrete HCG or Alpha Fetoprotein (AFP). The name ‘embryonal carcinoma’ reflects the appearance of the tumour cells, which resemble the cells normally seen in a developing embryo. Embryonal carcinoma is the most frequent tumour component of testicular mixed GCT, present in ~80% - 90% of cases. More than 90% of testicular neoplasms originate from germ cells. Testicular Germ Cell Tumours (GCTs) are a heterogeneous group of neoplasms with diverse histopathology and clinical behaviour. Average age of presentation 25 years - 35 years old, ~10 years younger than seminoma. Rare in children and adults over 50 years of age [1, 2].
Descent of the testicles is a necessary factor for proper testicular development. It has been observed that undescended testicles (cryptorchidism) are associated with about 10% of all germ cell tumours such as Embryonal Carcinoma of the testis. Undescended testicles (Cryptorchidism) are associated with decreased fertility (especially bilateral cases), increased testicular germ cell tumours (overall risk under 1%), testicular torsion, inguinal hernias, and psychological problems. Cryptorchidism is the absence of at least one testicle from the scrotum. It is the most common congenital defect involving male genitalia. About 3% of full-term and 30% of premature male infants are born with one or both testicles undescended. The testes normally descend by month 7 of gestation. Approximately 80% of cryptorchid testes descend by the third month of life after birth. This makes the true incidence around 1%. If the testis has not descended by six months of age, it is unlikely to do so spontaneously, and surgical correction should be considered [3, 4]. The undescended testicle can usually be palpated in the inguinal canal. In a minority of patients, the missing testicle may be located in the abdomen or be non-existent. About 20% to 30% of undescended testes are non-palpable. From 10% to 30% of patients with a unilateral undescended testis will develop infertility. This increases to 35% to 65% or more for bilateral disease. If bilateral cryptorchid testes are left untreated, the infertility rate increases to over 90% [5].
Case Report
One 43-year-old male patient presents at the emergency center, because of pain in the left inguinal region and a formation that is prominent to that body region. Tests were done and the results were normal, the abdominal surgeon was consulted, who notices a palpation and hard formation in the left inguinal region, which was grown, what rose the suspicion of an incarcerated inguinal hernia. The abdominal surgeon lists the patient for immediate surgical intervention, accessing through the inguinal region. Going through the layers, the formation was reached, which was when it was realized that we are dealing with a undescended testicle tumour. The urologist was called to the surgery room, who then discovers that we are dealing with a tumour of undescended testicle. The tumour was in the left undescended testicle. Left inguinal radical orchiectomy and mass biopsy were performed. Histopathological diagnosis revealed embryonal carcinoma. The testis with dimensions of 11.5 cm x 8 cm x 6.5 cm has been received.
In the macroscopic examination, on the surface of the cut, a relatively well-defined tumour formation can be observed, with a gray-yellow-pink color and a maximum diameter of 9.5 cm.
Histological description
The described tumour formation is made up of infiltrative islands and atypical-glandular structures, covered with neoplastic cells with an epithelial appearance. The neoplastic cells are medium in size, with amphophilic cytoplasm and vesicular nuclei with prominent nucleoli. There are foci and confluent areas of tumour necrosis. Foci of sclerosis and stromal hyalinization are also observed. There are foci of lympho-vascular invasion. The tunica albuginea is focally infiltrated (Figure 1).
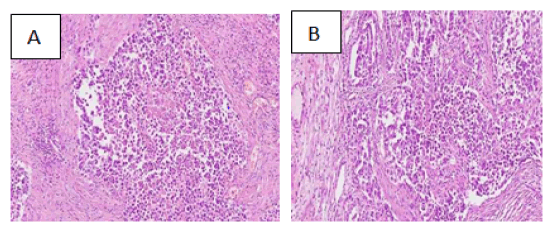
Figure 1: Microscopic images of Embryonal Carcinoma
The described tumour formation is made up of infiltrative islands and atypical-glandular structures, covered with neoplastic cells with an epithelial appearance. The neoplastic cells are medium in size, with amphophilic cytoplasm and vesicular nuclei with prominent nucleoli. There are foci and confluent areas of tumour necrosis.
Computed Tomographic (CT) scan showed multiple metastases: retroperitoneal lymph nodes mass and lungs and liver metastasis (Figure 2).
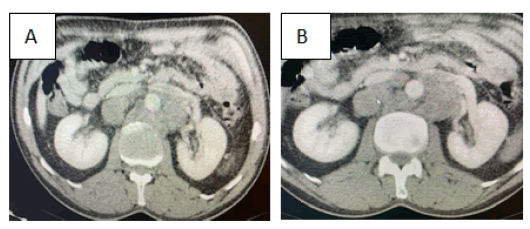
Figure 2: Computed tomographic (CT) scan showed: retroperitoneal lymph nodes (metastasis).
Tumour markers elevated; Beta HCG: 1432 mIU/mL, AFP: 409 ng/ml, LDH: 1007 U/L. Chemotherapy was started after 3 weeks from operation, with the Bleomycin, Etoposide, and Cisplatin (BEP) regimen, and this cycle was repeated every 3 weeks up to three times. After Chemotherapy the tumour markers results were as following: HCG: 4, AFP: 4.8, LDH: 450 U/L. After 3 months CT scan showed, the lungs and liver metastasis seem to have disappeared, and the retroperitoneal lymph nodes were decreased in size. Surgery performed within eight weeks after the last chemotherapy cycle. Retroperitoneal lymph nodes dissection was performed. Microscopic examination revealed no viable cancer cells. After retroperitoneal lymph nodes dissection, the tumour markers results were as following: HCG: 1.0, AFP: 3.6, LDH: 156 U/L. On CT scan, no retroperitoneal, liver, or lungs tumour was detected.
Discussion
The most common type of testis cancer is a Germ Cell Tumour (GCT). There are two main types of GCT: Non Seminomatous Germ Cell Tumours (NSGCT) and seminoma. Nonseminomatous germ cells tumours are: embryonal carcinoma, Yolk Sac Tumour (YST), choriocarcinoma, and teratoma. The etiology of GCTs is largely unknown. Cytogenetic studies suggest a different pathogenesis for each group of infantile/ prepubertal GCTs, postpubertal GCTs, and spermatocytic seminoma [1,6].
Embryonal carcinoma is the most common component in mixed GCTs. Eighty percent or more of embryonal carcinoma component and vascular invasion are recognized predictors of occult metastasis for clinical stage I mixed GCTs. Most patients with prepubertal yolk sac tumour, the most common pediatric GCT, have stage I disease at presentation. Most choriocarcinomas present with metastatic symptoms because of the propensity for rapid hematogenous dissemination [2,3,6].
Testicular germ cell tumours (GCTs) are a heterogeneous group of neoplasms with diverse histopathology and clinical behaviour. More than 90% of testicular neoplasms originate from germ cells Average age of presentation 25 years - 35 years old, ~10 years younger than seminoma. Rare in children and after 50 years of age. Embryonal carcinoma: present in about 40 percent of tumours and among the most rapidly growing and potentially aggressive tumour types. Embryonal carcinoma can secrete HCG or Alpha Fetoprotein (AFP) [4,5,10].
Descent of the testicles is a necessary factor for proper testicular development. It has been observed that undescended testicles (cryptorchidism) are associated with about 10% of all germ cell tumours such as Embryonal Carcinoma of the Testis. Undescended testicles are associated with decreased fertility (especially bilateral cases), increased testicular germ cell tumours (overall risk under 1%), testicular torsion, inguinal hernias, and psychological problems. [8,9,12].
Chemotherapy as initial treatment proved effective in a first-line setting (potentially even as dose-intensified therapy upfront) with data also supporting the use of multimodal treatment particularly in relapsed disease. Consolidation RT, even with total response after chemotherapy, should therefore be used in patients with brain metastases at relapse, but must be carefully discussed in a first-line s etting. S urgery m ay b e c onsidered i n c ases w ith a persistent solitary metastasis, depending on the systemic disease status, histology of the primary tumour and the location of the metastasis. Following first-line BEP only 6%-10% of residual masses contain active cancer, 50% post-pubertal teratoma, and 40% necrotic-fibrotic tissue only. Surgery, when indicated, should be performed within six to eight weeks after the last chemotherapy cycle. The role of surgery with residual retroperitoneal lesions < 1 cm is uncertain [12,13].
One 43-year-old male presents in Emergency with left inguinal pain and a mass in the inguinal region. The urologist was called to the surgery room, by abdominal surgeon, who then discovers that we are dealing with a tumour of undescended testicle. Left inguinal radical orchiectomy and mass biopsy were performed. Histopathological diagnosis revealed Embryonal carcinoma. Computed Tomographic (CT) scan showed multiple metastases: retroperitoneal lymph nodes, and lungs and liver metastasis. Tumour markers elevated; Beta HCG: 1432 mIU/mL, AFP: 409 ng/ml, LDH: 1007 U/L. Chemotherapy was started three weeks after the surrgery, with the Bleomycin, Etoposide, and Cisplatin (BEP) regimen, and this cycle was repeated three times, every three weeks, up to three times. After Chemotherapy the tumour markers results were as following: HCG: 4, AFP: 4.8, LDH: 450 U/L. After 3 months CT scan showed, the lungs and liver metastasis seem to have disappeared, and the retroperitoneal lymph nodes were decreased in size. After chemotherapy, retroperitoneal lymph nodes dissection was performed. Microscopic examination revealed no viable cancer cells. After retroperitoneal lymph nodes dissection, the tumour markers results were as following: HCG: 1.0, AFP:3.6, LDH: 156 U/L. On CT scan, no retroperitoneal, liver, or lungs tumour was detected.
Following first-line BEP only 6-10% of residual masses contain active cancer, 50% post-pubertal teratoma, and 40% necroticfibrotic tissue only. Surgery, when indicated, should be performed within six to eight weeks after the last chemotherapy cycle. The role of surgery with residual retroperitoneal lesions < 1 cm is uncertain [12,13]. It is difficult to distinguish between a true residual node below 10 mm and a complete remission, and many authors consider these situations as equivalent. Surgery is therefore indicated even with residual masses < 1 cm. When resection is indicated, bilateral nerve sparing RPLND is the standard option. Ipsilateral template resection avoids contralateral nerve dissection and may be considered for residuals with a diameter < 5 cm, as well as unilateral lymph node metastases on pre- and post-chemotherapy CT scans, left-sided tumours only require para-aortic resection whereas right-side tumours need paracaval and inter-aortocaval resection down to the iliac arteries. Following completion of treatment, cases with a low-level β-hCG plateau should be observed to determine whether complete normalisation subsequently occurs. In patients with a low plateau serum AFP level after chemotherapy, removal of residual masses should be undertaken, with subsequent AFP monitoring. Salvage chemotherapy is only indicated for documented marker progression [14-16].
Conclusion
Treatment of embryonal metastatic carcinoma with Chemotherapy: Bleomycin, Etoposide, and Cisplatin (BEP) and retroperitoneal lymph node dissection can be successful. In cases of early detection of the embryonal carcinoma, the treatment is easier and more successful and with a better prognosis for the patient. The grade, stage, size, histopathological of tumour are important prognostic indicators. Undescended testicle (cryptorchidism) is associated with increased testicular germ cell tumors such as Embryonal Carcinoma of the testis.
Conflict of Interest
The authors declare no conflict of interest or financial.
Funding
None
Author Contributions
All authors contributed to all stages of drafting this paper and, gave final approval of the version to be published.
References
- Guidelines on Testicular Cancer EAU, 2023, 05: 52
- Moch H, Amin M B , Berney D M, Compérat E A, Gill A J, et al. The 2022 World Health Organization Classification of Tumours of the Urinary System and Male Genital Organs-Part A: Renal, Penile, and Testicular Tumours. Eur Urol, 2022. 82: 458-468.
- Looijenga LH, Van der Kwast TH, Grignon D, Egevad L, Kristiansen G,et al. Report from the International Society of Urological Pathology (ISUP) consultation conference on molecular pathology of urogenital cancers: IV: current and future utilization of molecular-genetic tests for testicular germ cell tumors. Am j surg pathol. 2020 ;44:66-79.
- Lip SZ, Murchison LE, Cullis PS, Govan L, Carachi R. A meta-analysis of the risk of boys with isolated cryptorchidism developing testicular cancer in later life. Arch dis child. 2013;98:20-26.
- Del Giudice F, Kasman AM, De Berardinis E, Busetto GM, Belladelli F,et al. Association between male infertility and male-specific malignancies: systematic review and meta-analysis of population-based retrospective cohort studies. Fertil Steril. 2020 ;114:984-996.
- Brierley JD, Gospodarowicz MK. Wittekind Christian. TNM Classification of Malignant Tumours, 8th ed.; Wiley-Blackwell: Hoboken, NJ, USA. 2016.
- Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO classification of tumours of the urinary system and male genital organs—part A: renal, penile, and testicular tumours. European urology. 2016 Jul 1;70(1):93-105.[Google scholar][Cross ref]
- Gurney JK, Florio AA, Znaor A, Ferlay J, Laversanne M,et al. International trends in the incidence of testicular cancer: lessons from 35 years and 41 countries. Eur urol. 2019 ;76:615-623.
- Pluta J, Pyle LC, Nead KT, Wilf R, Li M,et al. Identification of 22 susceptibility loci associated with testicular germ cell tumors. Nat commun. 2021;12:4487.
- Park J.S, Kim J , Elghiaty A, Ham W S . Recent global trends in testicular cancer incidence and mortality. Medicine, 2018.97: 12390.
- Seikkula H, Hirvonen E, Kaipia A, Boström PJ, Malila N, et al. Familial aggregation of testicular cancer among early-onset cancer survivors. A prospective observational cohort data from Finland. Cancer Epidemiol. 2020 ;69:101807.
- Nason GJ, Jewett MA, Bostrom PJ, Goldberg H, Hansen AR,et al. Long-term surveillance of patients with complete response following chemotherapy for metastatic nonseminomatous germ cell tumor. Eur urol oncol. 2021;4:289-96.
- Ehrlich Y, Brames MJ, Beck SD, Foster RS, Einhorn LH. Long-term follow-up of cisplatin combination chemotherapy in patients with disseminated nonseminomatous germ cell tumors: is a postchemotherapy retroperitoneal lymph node dissection needed after complete remission?. J clin oncol. 2010 ;28:531-536.
- Gerdtsson A, Thor A, Bergdahl AG, Almås B, Håkansson U,et al. Unilateral or bilateral retroperitoneal lymph node dissection in nonseminoma patients with postchemotherapy residual tumour? Results from RETROP, a population-based mapping study by the Swedish Norwegian Testicular Cancer Group. Eur Urol Oncol. 2022;5:235-243.
- Beck SD, Foster RS, Bihrle R, Donohue JP, Einhorn LH. Is full bilateral retroperitoneal lymph node dissection always necessary for postchemotherapy residual tumor?. Cancer. 2007 ;110:1235-1240.
- Gerdtsson A, Thor A, Bergdahl AG, Almås B, Håkansson U,et al. Unilateral or bilateral retroperitoneal lymph node dissection in nonseminoma patients with postchemotherapy residual tumour? Results from RETROP, a population-based mapping study by the Swedish Norwegian Testicular Cancer Group. Eur Urol Oncol. 2022;5:235-243.



