Research - Onkologia i Radioterapia ( 2023) Volume 17, Issue 9
Sensitivity and specificity of ultrasound and mammography for detection of breast malignancy: A systematic review and metaanalysis
Neda Azarpey*Neda Azarpey, Department of Radiology, West Nikan Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran, Email: neda.azarpey.md@gmail.com
Received: 24-Jul-2023, Manuscript No. OAR-23-109112; Accepted: 25-Aug-2023, Pre QC No. OAR-23-109112(PQ); Editor assigned: 31-Jul-2023, Pre QC No. OAR-23-109112(PQ); Reviewed: 05-Aug-2023, QC No. OAR-23-109112(Q); Revised: 21-Aug-2023, Manuscript No. OAR-23-109112 (R); Published: 03-Sep-2023
Abstract
Background and Aim: In recent years, breast cancer is the most common cancer among women, and the average age of its occurrence is decreasing. Due to dense breast tissue in younger women, which reduces the sensitivity of mammography in the diagnosis of carcinoma. The use of ultrasound as a supplement to mammography is very useful in its diagnosis. Thus, this systematic review and meta-analysis is aimed at pooling the sensitivity and specificity of mammography and ultrasonography in detection of breast malignancy. Methods: We performed a systematic search of literature in PubMed, Web of Science, and Scopus with relevant keywords. Studies that did not perform ultrasound or mammography or did not perform any comparison were excluded. Data extraction was performed based on a standardized sheet. Pooling the sensitivities and specificities was performed with STATA, R, and RStudio. Results: The initial search retrieved 19,022 articles from which 8753 duplicates were removed. Finally, 28 studies were included based on our eligibility criteria. The pooled sensitivity of mammography in detection of breast malignancy was 78% (95% CI: 72% - 83%, p-value < 0.001). The pooled specificity of mammography in detection of breast malignancy was 78% (95% CI: 66% - 86%, p-value < 0.001). The pooled sensitivity of ultrasonography in detection of breast malignancy was 87% (95% CI: 80% - 92%, p-value < 0.001). The pooled specificity of ultrasonography in detection of breast malignancy was 75% (95% CI: 61% - 84%, p-value < 0.001). Conclusion: According to the findings of our study, ultrasonography had higher sensitivity for detection breast lesion malignancy compared to mammography, however, mammography showed higher specificity for detection of breast malignancy.
Keywords
breast cancer, ultrasound, ultrasonography, mammography, breast malignancy
Introduction
Today, breast cancer is one of the most common cancers and a common cause of death among women in the world. Breast tissue is dense in young people and gradually replaces dense breast tissue with age and fatty tissue. Despite the severe prognosis and high morbidity and mortality, the patient's prognosis will be better if diagnosed early. Early detection of breast cancer is the ultimate goal of radiology and the role of the radiologist is very crucial at this stage. Screening with mammography has caused a 22% decrease in the mortality of women over 50 years old and a 15% decrease in the mortality of women aged 40-49. Considering the incidence of breast cancer at younger ages in recent years and the presence of dense breast tissue in this group and the possibility of the lesion remaining hidden in this type of tissue, the existence of a complementary diagnostic method seems necessary to increase the sensitivity of diagnosis [1-4].
Primary randomized controlled trials have demonstrated the importance of mammography in early detection of breast cancer in asymptomatic women, with a 20-35% reduction in mortality, especially in women aged 50-69. It is shown. However, mammography-savvy women are still reluctant to undergo mammography because the cost is still prohibitive. In addition to economic problems, other difficulties also play a role. B. Fear of radiation, limited services available, anticipated pain, discomfort, fear of mammography for those in the know. Annual mammograms reportedly reduce breast cancer mortality in women over age 50 [5-9]. Hence, in this systematic review and meta-analysis study we aimed at pooling the sensitivity and specificity of mammography and ultrasonography in detection of breast malignancy
Methods and Materials
This systematic review and meta-analysis study was conducted based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline 2020 [1].
Search strategy
Two authors performed a systematic search of literature in the following electronic databases: PubMed, Web of Science, and Scopus. No time limitation was defined and all English studies from the beginning until June, 2023 were included. The relevant medical subject heading (MeSH) terms and related keywords were used in combination to build the search strategy; (“Ultrasound” OR “Mammography” OR “Ultrasonography” OR “US”) AND (“Breast Cancer” OR “Breast Neoplasm” OR “Breast Lesion”). More information regarding the search strategy is presented at Appendix 1.
Eligibility criteria
Our eligibility criteria were defined b ased o n t he P ICO framework: (P) Population: women suspected for breast cancer. (I) Not Applicable. (C) Ultrasound/Mammography findings. (O) Not applicable. Those studies that did not perform ultrasound or mammography or did not perform any comparison were excluded. Studies that performed MRI, lacked individual data, or were not in English, were also excluded.
Data extraction and outcome measures
A standardized Excel sheet was prepared for data extraction. Two independent authors performed the data extraction based on the aforementioned data extraction sheet. Disagreement between these two authors, regarding inclusion, exclusion or data extraction, was discussed and resolved by a third author. The data extraction sheet included the following study characteristics: first author’s name, year of publication, study design, true positive ultrasonography cases, true negative ultrasonography cases, false positive ultrasonography cases, false negative ultrasonography cases, true positive mammography cases, true negative mammography cases, false positive mammography cases, false negative mammography cases, total number of mammography cases, and total number of ultrasonography cases.
Data synthesis and statistical analysis
We used R (R Foundation for Statistical Computing, Vienna Austria), RStudio (RStudio, Inc., Boston, MA), and STATA 17.0 for the statistical analysis and creating the figures. The pooled sensitivity and specificity were calculated based on metadta package in STATA and mada package in R. The sensitivity and specificity were pooled using the hierarchical logistic regression. The 95% confidence interval was also estimated using the binomial distribution. The forest plots and receiver operating characteristic (SROC) plots were also created [10-12].
Results
Our initial search retrieved 19,022 articles from PubMed, Scopus, and Web of Science, from which 8753 duplicates were removed. After screening the title and abstract of 10,449 records, 51 full texts were retrieved, among which 28 studies were included based on our eligibility criteria (Figure 1)[13-40].
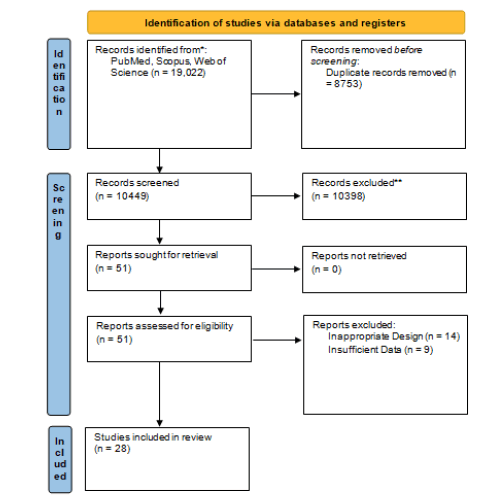
Figure 1: PRISMA flowchart of the included studies.
More detail regarding the study characteristics of the included studies is summarised in Tables 1 and 2.
Tab.1. Detailed characteristics of the included studies for mammography.
| Author | Year | Design | Age | TP | FP | FN | TN | Total |
|---|---|---|---|---|---|---|---|---|
| Ying et al. | 2012 | Retrospective Cohort Study | 46 | 201 | 61 | 45 | 358 | 665 |
| Wu et al. | 2016 | Prospective Cohort Study | 49 | 77 | 9 | 41 | 185 | 312 |
| Shao et al. | 2013 | Prospective Cohort Study | 53 | 40 | 13 | 15 | 22 | 90 |
| Mello et al. | 2017 | Retrospective Cohort Study | NA | 83 | 44 | 9 | 528 | 664 |
| Berg et al. | 2012 | Retrospective Cohort Study | NA | 57 | 414 | 18 | 4325 | 4814 |
| Habib et al. | 2009 | Retrospective Cohort Study | 36.5 | 11 | 4 | 1 | 4 | 20 |
| Lehman et al. | 2012 | Retrospective Cohort Study | 35 | 14 | 66 | 9 | 1119 | 1208 |
| Zahid et al. | 2009 | Retrospective Cohort Study | 35 | 40 | 6 | 12 | 152 | 210 |
| Yu et al. | 2016 | Retrospective Cohort Study | 48.2 | 127 | 40 | 41 | 79 | 287 |
| Ozulker et al. | 2010 | Prospective Cohort Study | NA | 13 | 5 | 3 | 8 | 29 |
| Omranipour et al. | 2016 | Prospective Cohort Study | 49.5 | 70 | 12 | 17 | 33 | 132 |
| Meissnitzer et al. | 2015 | Prospective Cohort Study | 50 | 57 | 18 | 10 | 7 | 92 |
| Tan et al. | 2014 | Retrospective Cohort Study | 40 | 36 | 28 | 38 | 224 | 326 |
| Cho et al. | 2016 | Retrospective Cohort Study | NA | 49 | 42 | 17 | 54 | 162 |
| Lee et al. | 2012 | Retrospective Cohort Study | 49.63 | 103 | 34 | 7 | 330 | 474 |
| Zhao et al. | 2015 | Retrospective Cohort Study | NA | 117 | 37 | 15 | 105 | 274 |
| Park et al. | 2014 | Retrospective Cohort Study | 49.6 | 24 | 14 | 18 | 62 | 118 |
| Yao et al. | 2014 | Retrospective Cohort Study | 35 | 374 | 27 | 104 | 1529 | 2034 |
| Novikov et al. | 2017 | Prospective Cohort Study | NA | 346 | 19 | 21 | 51 | 437 |
| Wang et al. | 2022 | Prospective Cohort Study | 35-70 | 1527 | 343 | 408 | 566 | 2844 |
| Mubuuke et al. | 2023 | Cross-sectional Study | 46.9 | 77 | 60 | 29 | 46 | 212 |
| Disha et al. | 2009 | Retrospective Cohort Study | 30-79 | 135 | 212 | 124 | 75 | 546 |
| Shafiq et al. | 2022 | Cross-sectional Study | 58.91 | 34 | 31 | 12 | 13 | 100 |
Tab.2. Detailed characteristics of the included studies for ultrasonography.
| Author | Year | Design | Age | TP | FP | FN | TN | Total |
|---|---|---|---|---|---|---|---|---|
| Barco et al. | 2016 | Retrospective Cohort Study | 58.5 | 162 | 76 | 180 | 1115 | 1533 |
| Habib et al. | 2009 | Retrospective Cohort Study | 36.5 | 12 | 3 | 2 | 5 | 22 |
| Lehman et al. | 2012 | Prospective Cohort Study | 35 | 22 | 128 | 1 | 1057 | 1208 |
| Sarica et al. | 2014 | Retrospective Cohort Study | 48 | 130 | 61 | 8 | 78 | 277 |
| Shao et al. | 2013 | Prospective Cohort Study | 53.2 | 44 | 14 | 11 | 21 | 90 |
| Ying et al. | 2012 | Retrospective Cohort Study | 50 | 235 | 82 | 11 | 337 | 665 |
| Wu et al. | 2016 | Retrospective Cohort Study | 49 | 32 | 3 | 86 | 191 | 312 |
| Zahid et al. | 2009 | Retrospective Cohort Study | 35 | 40 | 9 | 12 | 148 | 209 |
| Yu et al. | 2016 | Retrospective Cohort Study | 48.2 | 138 | 27 | 30 | 92 | 287 |
| Ozulker et al. | 2010 | Prospective Cohort Study | NA | 11 | 1 | 5 | 10 | 27 |
| Meissnitzer et al. | 2015 | Prospective Cohort Study | 50 | 66 | 20 | 1 | 5 | 92 |
| Vassiou et al. | 2009 | Prospective Cohort Study | 39 | 44 | 6 | 6 | 21 | 77 |
| Wang et al. | 2015 | Retrospective Cohort Study | 44 | 32 | 16 | 7 | 41 | 96 |
| Tan et al. | 2014 | Retrospective Cohort Study | 40 | 58 | 38 | 13 | 202 | 311 |
| Zhao et al. | 2015 | Retrospective Cohort Study | NA | 127 | 47 | 5 | 95 | 274 |
| Zhi et al | 2012 | Retrospective Cohort Study | 43 | 52 | 6 | 2 | 52 | 112 |
| Cho et al. | 2016 | Retrospective Cohort Study | NA | 58 | 19 | 8 | 77 | 162 |
| Lee et al. | 2012 | Retrospective Cohort Study | 49.63 | 108 | 47 | 2 | 317 | 474 |
| Park et al. | 2014 | Retrospective Cohort Study | 49.6 | 41 | 29 | 1 | 47 | 118 |
| Yao et al. | 2014 | Retrospective Cohort Study | 35 | 399 | 108 | 81 | 1148 | 1736 |
| Wang et al. | 2022 | Prospective Cohort Study | 35-70 | 1851 | 519 | 84 | 390 | 2844 |
| Mubuuke et al. | 2023 | Cross-sectional Study | 46.9 | 73 | 55 | 33 | 51 | 212 |
| Disha et al. | 2009 | Retrospective Cohort Study | 30-79 | 188 | 254 | 71 | 33 | 546 |
| Shafiq et al. | 2022 | Cross-sectional Study | 58.91 | 39 | 37 | 17 | 7 | 100 |
The pooled sensitivity of mammography in detection of breast malignancy was 78% (95% CI: 72% - 83%, p-value < 0.001). The pooled specificity of mammography in detection of breast malignancy was 78% (95% CI: 66% - 86%, p-value < 0.001). Further detail is available in Figures 2 and 3.
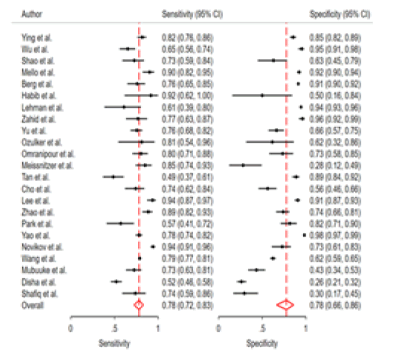
Figure 2: Pooled sensitivity and specificity of mammography.
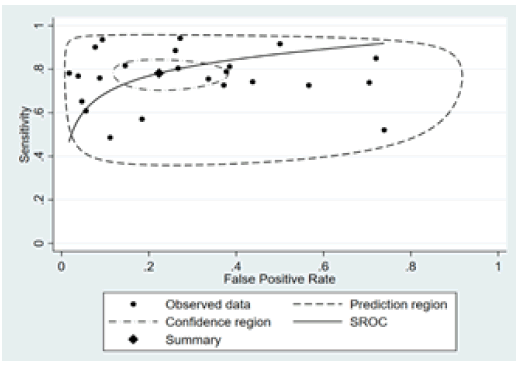
Figure 3: The receiver operating characteristic plot of mammography.
The pooled sensitivity of ultrasonography in detection of breast malignancy was 87% (95% CI: 80% - 92%, p-value < 0.001). The pooled specificity of ultrasonography in detection of breast malignancy was 75% (95% CI: 61% - 84%, p-value < 0.001). Further detail is available in Figures 4 and 5.
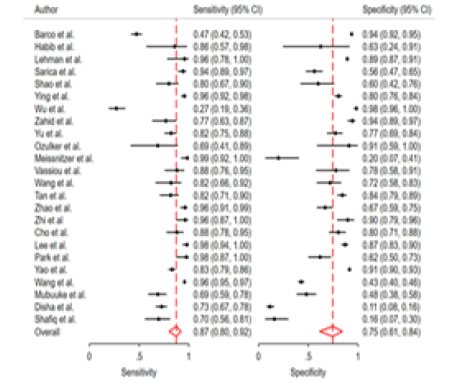
Figure 4: Pooled sensitivity and specificity of ultrasonography.
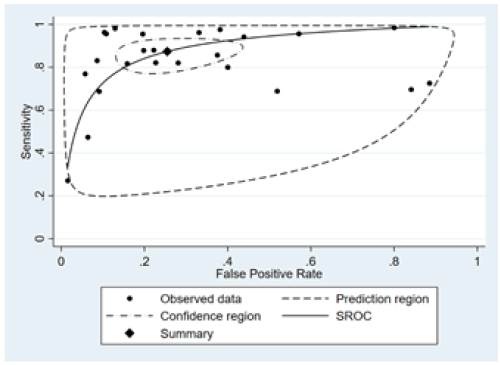
Figure 5: The receiver operating characteristic plot of ultrasonography.
Discussion
Based on the findings of our systematic review and meta-analysis study, ultrasonography had higher sensitivity for detection breast lesion malignancy compared to mammography, however, mammography showed higher specificity for detection of breast malignancy.
The challenge is determining which method is suitable for screening. Current imaging guidelines recommend mammography as the gold standard for imaging, especially for women over the age of 40. However, mammography has some limitations. For example, sensitivity is significantly lower in women with dense breasts, but such women have an increased risk of developing breast cancer. This is despite having automated systems to support diagnostics. B. A computerized system that allows superior performance compared to human readers, even in dense breasts
during mammography. Based on the results of this study, it can be argued that the addition of ultrasound to breast cancer screening procedures is more likely to result in better detection and early patient treatment. Previous literature supports this observation [41-46].
The use of breast ultrasound becomes even more important in lowincome areas where mammography machines are not available or where formal national mammography screening procedures are not available to all women. One reason for this is the enormous costs associated with establishing routine mammography screening procedures. Therefore, breast ultrasound may be promoted as an evaluation tool because it is relatively accessible and more affordable in low-income settings. The use of ultrasound as an adjunct to mammography in breast cancer screening continues to provoke controversy, mainly due to its low PPV and likely high NPV. Therefore, further studies in different contexts are needed to contribute to these discussions [47-49].
The use of BI-RADS systems to characterize breast tumors is recommended in many settings, and such reporting systems may help distinguish between benign and malignant breast tumors. The accuracy of BI-RADS systems remains controversial, and further research is needed in many areas to provide evidence on how accurate BI-RADS is in practice. The results of this study indicate that his PPV rate of BI-RADS 3–5 is high. This could bring light to the end of the tunnel. The use of BI-RADS has the potential to distinguish between benign and malignant masses, reducing unnecessary biopsies as well as unnecessary surgeries. This observation has already been pointed out in previous literature. The risk of BI-RADS 3 malignancies is less than 2% and most physicians recommend observation only for this category of patients. Although BI-RADS 4 breast tumors are classically nonmalignant, there is sufficient suspicion for core biopsy, whereas BIRADS 5 masses are at high risk of malignancy and warrant biopsy. there is [50-52].
When imaging suspicious breast lesions, there are other factors that affect imaging accuracy. For example, patient age, surgical history, characteristics of the lesion itself, menstrual and menopausal status, imaging techniques and protocols, use of newer technologies such as vacuum-assisted breast biopsy techniques, and imaging equipment used. All of these must be considered when using image accuracy results. A major limitation of this study is that breast density was not considered in the analysis and may play an important role. It is therefore recommended that future studies addressing breast density consider breast density. We also did not perform age-related sub-analyses to compare results for women under 40 years of age and those over 40 years of age. Therefore, we recommend future studies to investigate this aspect. Furthermore, further studies on the accuracy of breast ultrasound and her BIRADS in other settings are encouraged to further improve the evidence for considering these aspects in breast cancer screening [1, 53-55].
Conclusion
In conclusion, our systematic review and meta-analysis aimed to consolidate data on the sensitivity and specificity of both mammography and ultrasonography in the detection of breast malignancies. Our study findings reveal that ultrasonography demonstrated higher sensitivity in detecting breast lesion malignancies when compared to mammography. However, it's noteworthy that mammography exhibited greater specificity in the detection of breast malignancies.
References
- Vy VPT, Yao MM-S, Khanh Le NQ, Chan WP. Machine Learning Algorithm for Distinguishing Ductal Carcinoma In Situ from Invasive Breast Cancer. Cancers. 2022;14:2437.[Google Scholar] [Crossref]
- Balkenende L, Teuwen J, Mann RM, editors. Application of deep learning in breast cancer imaging. Seminars in Nuclear Medicine. 2022;52:291-301. [Google Scholar] [Crossref]
- Taylor DB, Burrows S, Saunders CM, Parizel PM, Ives A. Contrast-enhanced mammography (CEM) versus MRI for breast cancer staging: detection of additional malignant lesions not seen on conventional imaging. Eur Radiol Exp. 2023;7:8. [Google Scholar] [Crossref]
- Lobig F, Caleyachetty A, Forrester L, Morris E, Newstead G, Harris J, et al. Performance of supplemental imaging modalities for breast cancer in women with dense breasts: findings from an umbrella review and primary studies analysis. Clin Breast Cancer. 2023;23:e55-e65. [Google Scholar] [Crossref]
- Sardini B, Fogh Jørgensen S, Brønsro Larsen L, Elhakim MT, Njor SH. Choice of Assessment and Subsequent Risk of Breast Cancer among Women with False-Positive Mammography Screening. Cancers. 2023;15:1867. [Google Scholar] [Crossref]
- Joshi P, Singh N, Raj G, Singh R, Malhotra KP, Awasthi NP. Performance evaluation of digital mammography, digital breast tomosynthesis and ultrasound in the detection of breast cancer using pathology as gold standard: an institutional experience. Egypt J Radiol Nucl Med. 2022;53:1-11. [Google Scholar] [Crossref]
- Lohitvisate W, Pummee N, Kwankua A. Mammographic and ultrasonographic features of triple-negative breast cancer compared with non-triple-negative breast cancer. J Ultrasound. 2023;26:193-200. [Google Scholar] [Crossref]
- Monticciolo DL, Newell MS, Moy L, Lee CS, Destounis SV. Breast Cancer Screening for Women at Higher-Than-Average Risk: Updated Recommendations From the ACR. J Am Coll Radiol. 2023. [Google Scholar] [Crossref]
- Prodan M, Paraschiv E, Stanciu A. Applying Deep Learning Methods for Mammography Analysis and Breast Cancer Detection. Appl Sci. 2023;13:4272. [Google Scholar] [Crossref]
- Nyaga VN, Arbyn M. Metadta: a Stata command for meta-analysis and meta-regression of diagnostic test accuracy data – a tutorial. Arch Public Health. 2022;80:95. [Google Scholar] [Crossref]
- Harbord RM, Whiting P. Metandi: meta-analysis of diagnostic accuracy using hierarchical logistic regression. Stata J. 2009;9:211-29. [Google Scholar] [Crossref]
- Doebler P, Holling H. Meta-analysis of diagnostic accuracy with mada. R Package. 2015;1:15. [Google Scholar] [Crossref]
- Barco I, Chabrera C, García-Fernández A, Fraile M, González S, et al. Role of axillary ultrasound, magnetic resonance imaging, and ultrasound-guided fine-needle aspiration biopsy in the preoperative triage of breast cancer patients. Clin Transl Oncol. 2017;19:704-710. [Google Scholar] [Crossref]
- Berg WA, Madsen KS, Schilling K, Tartar M, Pisano ED, et al. Comparative effectiveness of positron emission mammography and MRI in the contralateral breast of women with newly diagnosed breast cancer. AJR Am J Roentgenol. 2012;198(1):219-232. [Google Scholar] [Crossref]
- Cho MJ, Yang JH, Yu YB, Park KS, Chung HW, et al. Validity of breast-specific gamma imaging for Breast Imaging Reporting and Data System 4 lesions on mammography and/or ultrasound. Ann Surg Treat Res. 2016;90:194-200. [Google Scholar] [Crossref]
- Devolli-Disha E, Manxhuka-Kërliu S, Ymeri H, Kutllovci A. Comparative accuracy of mammography and ultrasound in women with breast symptoms according to age and breast density. Bosn J Basic Med Sci. 2009;9:131-136. [Google Scholar] [Crossref]
- Habib S, Maseeh uz Z, Hameed A, Niaz K, Hashmi H, et al. Diagnostic accuracy of Tc-99m-MIBI for breast carcinoma in correlation with mammography and sonography. J Coll Physicians Surg Pak. 2009;19:622-626. [Google Scholar] [Crossref]
- Lee A, Chang J, Lim W, Kim BS, Lee JE, et al. Effectiveness of breast-specific gamma imaging (BSGI) for breast cancer in Korea: a comparative study. Breast J. 2012;18(5):453-48. [Google Scholar] [Crossref]
- Lehman CD, Lee CI, Loving VA, Portillo MS, Peacock S,et al. Accuracy and value of breast ultrasound for primary imaging evaluation of symptomatic women 30-39 years of age. Am J Roentgenol. 2012;199:1169-1177. [Google Scholar] [Crossref]
- Meissnitzer T, Seymer A, Keinrath P, Holzmannhofer J, Pirich C, et al. Added value of semi-quantitative breast-specific gamma imaging in the work-up of suspicious breast lesions compared to mammography, ultrasound and 3-T MRI. Br J Radiol. 2015;88(1051):20150147. [Google Scholar] [Crossref]
- Mello J, Bittelbrunn FP, Rockenbach M, May GG, Vedolin LM, et al. Breast cancer mammographic diagnosis performance in a public health institution: a retrospective cohort study. Insights Imaging. 2017;8:581-588. [Google Scholar] [Crossref]
- Mubuuke AG, Nassanga R, Galukande M. Comparative accuracy of sonography, mammography and the BI-RADS characterization of breast masses among adult women at Mulago Hospital, Uganda. J Glob Health Rep. 2023;7:e2023013. [Google Scholar] [Crossref]
- Novikov S, Kanaev S, Chernaya A, Krzhivitskiy P, Krivorotko P, et al. Diagnostic accuracy of mammography and scintimammography with 99m Tc-MIBI in detection of early breast cancer. 2017. [Google Scholar]
- Omranipour R, Kazemian A, Alipour S, Najafi M, Alidoosti M, et al. Comparison of the Accuracy of Thermography and Mammography in the Detection of Breast Cancer. Breast Care (Basel). 2016;11:260-264. [Google Scholar] [Crossref]
- Ozülker T, Ozülker F, Ozpaçaci T, Bender O, DeÄ?irmenci H. The efficacy of (99m)Tc-MIBI scintimammography in the evaluation of breast lesions and axillary involvement: a comparison with X-ray mammography, ultrasonography and magnetic resonance imaging. Hell J Nucl Med. 2010;13:144-149. [Google Scholar] [Crossref]
- Park KS, Chung HW, Yoo YB, Yang JH, Choi N, et al. Complementary role of semiquantitative analysis of breast-specific gamma imaging in the diagnosis of breast cancer. Am J Roentgenol. 2014;202:690-695. [Google Scholar] [Crossref]
- Sarica O, Uluc F. Additional diagnostic value of MRI in patients with suspicious breast lesions based on ultrasound. Br J Radiol. 2014;87:20140009. [Google Scholar] [Crossref]
- Shafiq M. Diagnostic Accuracy of Mammography Versus Ultrasound in Prediction of Malignancy with Palpable Breast Lesion. Pak J Med Dent. 2022;11:11-16. [Google Scholar] [Crossref]
- Shao H, Li B, Zhang X, Xiong Z, Liu Y, et al. Comparison of the diagnostic efficiency for breast cancer in Chinese women using mammography, ultrasound, MRI, and different combinations of these imaging modalities. J Xray Sci Technol. 2013;21(2):283-292. [Google Scholar] [Crossref]
- Tan K, Rumaisa M, Radhika S, Nurismah M, Norlia A, et al. The comparative accuracy of ultrasound and mammography in the detection of breast cancer. Med J Malaysia. 2014;69:79-85. [Google Scholar] [Crossref]
- Vassiou K, Kanavou T, Vlychou M, Poultsidi A, Athanasiou E, et al. Characterization of breast lesions with CE-MR multimodal morphological and kinetic analysis: comparison with conventional mammography and high-resolution ultrasound. Eur J Radiol. 2009;70:69-76. [Google Scholar] [Crossref]
- Wang J, Chen H, Wu X, Tang L. Comparison of diagnostic efficiency of breast cancer imaging in Chinese women: Digital mammography, ultrasound, MRI, and combinations of these modalities. J Med Imaging Health Inform. 2015;5:1488-1493. [Google Scholar] [Crossref]
- Wang Y, Li Y, Song Y, Chen C, Wang Z, et al. Comparison of ultrasound and mammography for early diagnosis of breast cancer among Chinese women with suspected breast lesions: A prospective trial. Thorac Cancer. 2022;13:3145-3151. [Google Scholar] [Crossref]
- Wu X, Lin Q, Lu J, Chen G, Zeng YI et al. Comparison of mammography and ultrasound in detecting residual disease following bioptic lumpectomy in breast cancer patients. Mol Clin Oncol. 2016;4:419-424. [Google Scholar] [Crossref]
- Yao X, Wei W, Li J, Wang L, Xu Z, et al. A comparison of mammography, ultrasonography, and far-infrared thermography with pathological results in screening and early diagnosis of breast cancer. Asian Biomed. 2014;8:11-19. [Google Scholar] [Crossref]
- Ying X, Lin Y, Xia X, Hu B, Zhu Z,et al. A comparison of mammography and ultrasound in women with breast disease: A receiver operating characteristic analysis. Breast J. 2012;18(2):130-138. [Google Scholar] [Crossref]
- Yu X, Hu G, Zhang Z, Qiu F, Shao X, et al. Retrospective and comparative analysis of (99m)Tc-Sestamibi breast specific gamma imaging versus mammography, ultrasound, and magnetic resonance imaging for the detection of breast cancer in Chinese women. BMC Cancer. 2016;16:450. [Google Scholar] [Crossref]
- Zahid Z, Ibrahim Z, Bilal S, Farooq M. Comparison of Diagnostic Accuracy of Film-Screen Mammography and Ultrasound in Breast Masses. PJMHS. 2011;5:433-435. [Google Scholar] [Crossref]
- Zhao H, Zou L, Geng X, Zheng S. Limitations of mammography in the diagnosis of breast diseases compared with ultrasonography: A single-center retrospective analysis of 274 cases. Eur J Med Res. 2015;20:1-7. [Google Scholar] [Crossref]
- Zhi W, Gu X, Qin J, Yin P, Sheng X, et al. Solid breast lesions: Clinical experience with US-guided diffuse optical tomography combined with conventional US. Radiology. 2012;265:371-378. [Google Scholar] [Crossref]
- Jalalian A, Mashohor SB, Mahmud HR, Saripan MIB, Ramli ARB, et al. Computer-aided detection/diagnosis of breast cancer in mammography and ultrasound: A review. Clin Imaging. 2013;37:420-426. [Google Scholar] [Crossref]
- Aristokli N, Polycarpou I, Themistocleous S, Sophocleous D, Mamais I. Comparison of the diagnostic performance of Magnetic Resonance Imaging (MRI), ultrasound and mammography for detection of breast cancer based on tumor type, breast density and patient's history: A review. Radiography. 2022. [Google Scholar] [Crossref]
- Coffey K, Jochelson MS. Contrast-enhanced mammography in breast cancer screening. Eur J Radiol. 2022:110513. [Google Scholar] [Crossref]
- Sahu A, Das PK, Meher S. High accuracy hybrid CNN classifiers for breast cancer detection using mammogram and ultrasound datasets. Biomed Signal Process Control. 2023;80:104292. [Google Scholar] [Crossref]
- Baek SJ, Ko KH, Jung HK, Park AY, Koh J. Comparison of abbreviated MRI with mammography and ultrasound in women with a personal history of breast cancer. Acad Radiol. 2022;29:19-25. [Google Scholar] [Crossref]
- DoÅ?Ä?ga-Kozierowski B, Lis M, Marszalska-Jacak H, Koziej M, Celer M, et al. Multimodality imaging in lobular breast cancer: Differences in mammography, ultrasound, and MRI in the assessment of local tumor extent and correlation with molecular characteristics. Front Oncol. 2022;12:855519. [Google Scholar] [Crossref]
- Wang Y, Li Y, Song Y, Chen C, Wang Z, et al. Comparison of ultrasound and mammography for early diagnosis of breast cancer among Chinese women with suspected breast lesions: A prospective trial. Thorac Cancer. 2022;13:3145-3151. [Google Scholar] [Crossref]
- Sriussadaporn S, Sriussadaporn S, Pakâ?art R, Kritayakirana K, Prichayudh S, et al. Ultrasonography increases sensitivity of mammography for diagnosis of multifocal, multicentric breast cancer using whole breast histopathology as a gold standard. Surg Pract. 2022;26:181-186. [Google Scholar] [Crossref]
- Ban K, Tsunoda H, Togashi S, Kawakami M, Takei J, et al. Comparative study of the usefulness of adjunctive tomosynthesis in breast cancer screening by mammography and ultrasound in Japan. Breast Cancer. 2022;29:790-795. [Google Scholar] [Crossref]
- Mann RM, Athanasiou A, Baltzer PA, Camps-Herrero J, Clauser P, et al. Breast cancer screening in women with extremely dense breasts: Recommendations of the European Society of Breast Imaging (EUSOBI). Eur Radiol. 2022;32:4036-4045. [Google Scholar] [Crossref]
- Ma M, Liu R, Wen C, Xu W, Xu Z, Wang S, et al. Predicting the molecular subtype of breast cancer and identifying interpretable imaging features using machine learning algorithms. Eur Radiol. 2022:1-11. [Google Scholar] [Crossref]
- Laçi I, Bërdica L, Nina H, Akshija I, Spahiu A, et al. The diagnostic value of ultrasound and mammography in detection of breast cancer in Albania. Int J Public Health. 2023;12:427-436. [Google Scholar]| [Crossref]
- Shah SM, Khan RA, Arif S, Sajid U. Artificial intelligence for breast cancer analysis: Trends & directions. Comput Biol Med. 2022:105221. [Google Scholar] [Crossref]
- Pulappadi VP, Dhamija E, Baby A, Mathur S, Pandey S, et al. Imaging Features of Breast Cancer Subtypes on Mammography and Ultrasonography: An analysis of 479 patients. Indian J Surg Oncol. [Google Scholar] [Crossref]
- Muduli D, Dash R, Majhi B. Automated diagnosis of breast cancer using multi-modal datasets: A deep convolution neural network based approach. Biomed Signal Process Control. 2022;71:102825.[Google Scholar] [Crossref]



