Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 4
Postoperative hypothermia in cancerous patients undergoing oncological surgery receiving general anesthesia
Ibrahem Ghaleb Ibrahem*Ibrahem Ghaleb Ibrahem, Department of anesthetic technique, Al-farahidi University, Collage of Medical Technology, Baghdad, Iraq, Tel: +964 770 580 6783, Email: m31947683@gmail.com
Received: 11-Apr-2023, Manuscript No. OAR-23-92493; Accepted: 29-Apr-2023, Pre QC No. OAR-23-92493 (PQ); Editor assigned: 13-Apr-2023, Pre QC No. OAR-23-92493 (PQ); Reviewed: 25-Apr-2023, QC No. OAR-23-92493 (Q); Revised: 28-Apr-2023, Manuscript No. OAR-23-92493 (R); Published: 30-Apr-2023
Abstract
Hypothermia is the temperature degree below 36°C, and it is a common problem during general surgery. Extremes age groups are more exposed to perioperative hypothermia. This study described postoperative hypothermia in cancerous patients receiving general anesthesia. A retrospective study was conducted, using anesthetic reports of temperature changing through surgery and in the post-anesthesia period in cancerous patients who had undergone general surgery at June 2020 and January 2023. Two hundred patients were enrolled in this work. All patients receiving general anesthesia depending on each operations protocol. Demographic and clinical variables data were collected including age, BMI, duration of anesthesia, and amount of irrigation fluid. A tympanic thermometer (BRAUN, China) was used to measured body temperatures. The body temperatures at the time of admission, at induction of anesthesia, one hour after general anesthesia, postoperative, at waken room and one hour later were 37.0 ± 0.2°C, 36.8 ± 0.4°C, 35. 9 ± 0.3°C, 35. 7 ± 0.3°C, 35.9 ± 0.2°C and 35.9 ± 0.4°C, respectively. The incidence of hypothermia was 76.5% while normothermia was 23.5%, documenting a significant difference (X2-test= 20.07, P < 0.001). The severity of hypothermia was significantly different between the groups (X2-test= 15.33, P<0.01). The incidence of postoperative hypothermia is high. The temperature dropping is more prominent and gradually happen throughout surgical procedures. Further warming methods required to prevent postoperative hypothermia during surgery.
http://www.oajournal.org/
http://www.journalsres.org/
http://www.journalsres.com/
http://www.journalsoa.org/
http://www.journalsoa.com/
http://www.journalsci.org/
http://www.journalres.org/
http://www.journalres.com/
http://www.journaloa.org/
http://www.journalinsights.org/
http://www.jpeerreview.org/
http://www.imedresearch.com/
http://www.imedpubjournals.com/
http://www.imedpubjournal.org/
http://www.imedjournals.org/
http://www.peerreviewedjournal.org/
http://www.peerjournals.org/
http://www.peerjournals.com/
http://www.sciencesinsight.org/
http://www.scholarresearch.com/
http://www.scholarres.org/
http://www.nutritionres.com/
http://www.gastroinsights.org/
http://www.pathologyinsights.org/
http://www.echemistry.org/
http://www.echemcentral.com/
http://www.chemistryres.com/
http://www.biochemresearch.org/
http://www.biochemjournals.com/
http://www.ebusinessjournals.org/
http://www.businessjournals.org/
http://www.peerjournal.org/
http://www.oajournalres.com/
http://www.alliedres.org/
http://www.alliedjournals.org/
http://www.alliedjournal.org/
http://www.scientificres.org/
http://www.scientificres.com/
,
https://www.mongoliannutrition.com/
https://www.nsbmb.com/
https://www.arabspp.org/
https://www.arabianmultidisciplinary.com/
https://www.italystemcell.com/
https://www.traditional-medicine.org/
https://www.episportsmedicine.org/
https://www.worldmedicalassociation.org/
https://www.silaeitaly.com/
https://www.ceramicsmedicine.org/
https://www.isaddictionmedicine.org/
https://www.europeanbionetwork.com/
https://www.aarsecp.com/
https://www.edycseg.org/
https://www.europeanneurology.org/
https://www.clinicaldermepi.com/
https://www.cardiac-society.com/
https://www.psychologicalassociation.org/
https://www.indian-psychology.com/
https://www.mongoliancardiology.org/
https://www.pediatricssociety.com/
https://www.cocrt.org/
https://www.european-aesthetic.com/
https://www.sohnsb.org/
Keywords
Post-surgery, general anesthesia, hypothermia, heat loss, oncological surgery
Introduction
Hypothermia, is a core temperature below 36°C, occur in patients undergoing general surgery due to heat loss as a result of the large amounts administration of the irrigation fluid of the room temperature [1–4]. Perioperative hypothermia leads to several problems like morbid cardiac sequel [5], DIC coagulopathy and increased transfusion requirements [6], infections of surgical wound [7], and prolongation of the recovery postoperatively [8].
Patients with extreme age groups have a great risk of intraoperative and post-operative hypothermia due to less ability to control own body temperature [9, 10].
The aim of this study described postoperative hypothermia in patients receiving general anesthesia.
Methodology
Study design and setting
A retrospective analysis was conducted, using anesthetic reports of body temperature changing through surgery and in the postanesthesia period in cancerous patients who had undergone general surgery at June 2020 and January 2023. Two hundred patients were enrolled in this work.
Ethical approval
Institutional Review Board of Hospital approved this study (#10, 2022).
Anesthesia protocol
All patients receiving general anesthesia using ropivacaine and postoperative pain control prior to anesthesia, depending on each operations protocol. Induction done with propofol, and fentanyl, then intubation done. The maintenance with desflurane and a 50% nitrous oxide in oxygen mixture was applied.
Data collection
Demographic and clinical variables data were collected including age, BMI, cancer types, surgery types, duration of anesthesia, and amount of irrigation fluid. A tympanic thermometer (BRAUN, China) was used to measured body temperatures. The temperature values investigated were:
1. At admission
2. At induction of anesthesia
3. One hour after general anesthesia
4. Post operation
5. At recovery room
6. One hour later
The hypothermia degree was divided into:
1. Mild : 35.5–35.9°C
2. Moderate : 35.0–35.4°C
3. Severe : 34.5–34.9°C
Statistical Analysis
The data thus obtained was analyzed using descriptive statistics. SPSS v 24 (IBM Inc., Chicago, IL, USA) was used. Mean, median, and SD for categorical data calculated. An X2 test used for the categorical variables. A P value <0.05 was considered significant.
Results
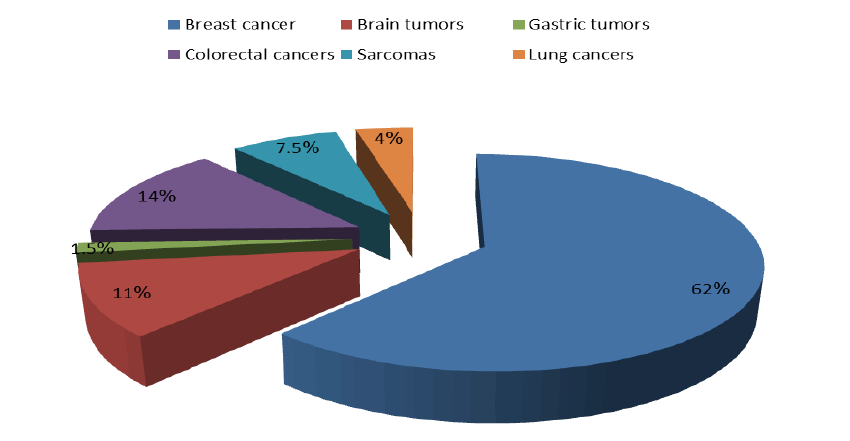
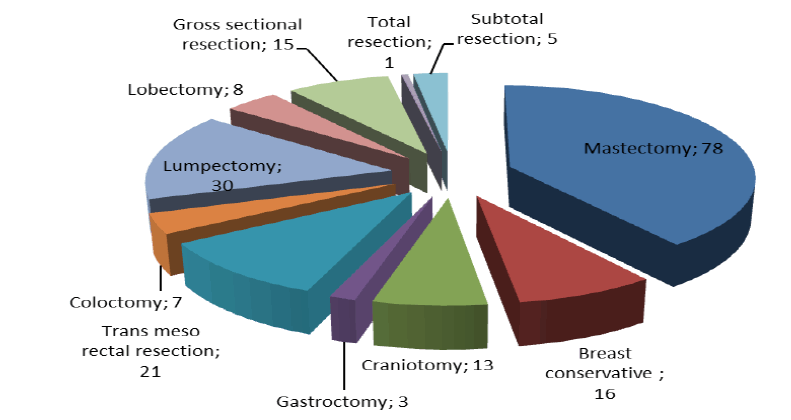
Patient and peri and postoperative data including age, BMI, duration of anaesthesia and surgery and amount of irrigation fluid were recorded (Table 1). The distribution of cancer types figured in (Figure 1). The oncological surgery types figured in (Figure 2). The body temperatures at the time of admission, at induction of anaesthesia, one hour after general anaesthesia, postoperative, at recovery room and one hour later were 37.0 ± 0.2°C, 36.8 ± 0.4°C, 35. 9 ± 0.3°C, 35. 7 ± 0.3°C, 35.9 ± 0.2°C and 35.9 ± 0.4°C, respectively, with a high significant difference (Table 2). The incidence of hypothermia was 76.5% while normothermia was 23.5%, documenting a significant difference (X2 -test= 20.07, P < 0.001). The severity of hypothermia was significantly different between the groups (X2 -test= 15.33, P<0.01); severe hypothermia was observed in 26.8% (Table 3 and 4).
Tab. 1. Patient and peri and postoperative data
| Variables | Mean ± SD |
|---|---|
| Age (year) | 59.3 ± 10.4 |
| BMI (k/m2) | 35.6 ± 4.8 |
| Anesthesia duration (min) | 111.2 ± 25.5 |
| Operation duration (min) | 67.1 ± 20.2 |
| Irrigation fluid (L) | 33.9 ± 12.6 |
Figure 1: The distribution of cancer types
Figure 2:Oncological surgery types
Tab. 2. Body temperature measurement
| Temperature | Mean ± SD |
|---|---|
| At admission | 37.0 ± 0.2 |
| At induction of anesthesia | 36.8 ± 0.4 |
| One hour after general anesthesia | 35. 9 ± 0.3 |
| Postoperative | 35. 7 ± 0.3 |
| At recovery room | 35.9 ± 0.2 |
| One hour late | 35.9 ± 0.4 |
Tab. 3. Incidence of hypothermia
| Thermia (n = 200) | No. | % |
|---|---|---|
| Normothermia | 47 | 23.5 |
| Hypothermia | 153 | 76.5 |
X2 -test= 20.07, P<0.001
Tab. 4. Severity of hypothermia
| Severity (n=153) | No. | % |
|---|---|---|
| Mild | 79 | 51.6 |
| Moderate | 33 | 21.6 |
| Severe | 41 | 26.8 |
X2 -test= 15.33, P<0.01
Discussion
In this study, postoperative hypothermia has a higher incidence (76.5%) of. In addition, the body temperature was dropped gradually from point of admission till time of operation room, recovery room and event at postoperative period. Most of patients underwent general anaesthesia are prone to hypothermia as a result of anaesthetic-induced impairment of thermoregulatory control, impaired thermoregulatory vasoconstriction and exposure to a cold operating room [9, 10].
Guidelines by the British National Institute for Health and Care Excellence was present steps for the prevention of perioperative hypothermia including: The patient’s temperature measured before the induction of anaesthesia and then every 1/2 hour until post-surgery, kept the ambient temperature above 21°C, warming of intravenous fluids and blood products performing, and a forced-air warming device using if the temperature decline below 36°C [11].
In the present study, the amount of irrigation fluid administered is consistent with the findings reported by Kim et al [4], in that the core body temperature is correlated with patient age in cases.
The benefit of forced-air warming system to reduce radiating heat loss by replacing the cool room environment with a warm cover. Beside, a forced-air warming system preventing decline in the temperature by producing a flow of warm air pass the skin and by enhancing convection to raise heat gain [12].
The pre-warming prior to surgery may prevent the dropping in core temperature through re-distribution of body heat between the core and peripheral tissues [13].
In the present study, the severe hypothermia was 26.8%; moderate was 21.6% and mild was 51.6%. These findings support the previous findings that patients become more hypothermic during surgery [10, 14, 15]
Lim et al [16], prevented intra-operative hypothermia through surgery by lowering the intra-operative concentration of anaesthetic drugs prior to surgery.
In the present study, the incidence of hypothermia was 76.5%, lower than that reported in the study of Kim et al, as (91.3%) [4].
Some authors have reported that warmed fluid irrigation during orthopedic surgery declined the rate of hypothermia [1, 4], whereas finding noticed that warmed fluid irrigation not prevent development of hypothermia post-surgery [3].
In Iraq, several limitations lead to these findings of this study. First, the operating room temperature and general anesthetics were not well evaluated. Second, the way of temperature recovering of the patients in the waken room was not documented sufficiently. Third, there are no standard criteria and guidelines were setting in this nationality. Fourth, low socio-economic and educated levels of patients undergoing surgery. Lastly, moderately training in surgical theatres staff including surgeon and anaesthetics assistants regarding hypothermia complication postoperatively.
Conclusion
The incidence of postoperative hypothermia is high. The temperature dropping is more prominent and gradually happen throughout surgical procedures. Further warming methods required to prevent postoperative hypothermia during surgery.
Conflict of Interest
None
FUNDING SUPPORTING
None.
References
- Jin Y, Tian J, Sun M, Yang K. A systematic review of randomised controlled trials of the effects of warmed irrigation fluid on core body temperature during endoscopic surgeries. J Clin Nurs. 2011;20:305-316.
- Lee JJ, Choi GJ, Lee WJ, Choi SB, Kang H. Effect of active airway warming with a heated-humidified breathing circuit on core body temperature in patients under general anesthesia: a systematic review and meta-analysis with trial sequential analysis. Korean J Anesthesiol. 2022.
- Campbell G, Alderson P, Smith AF, Warttig S. Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. 2015.
- Kim YS, Lee JY, Yang SC, Song JH, Koh HS, et al. Comparative study of the influence of room-temperature and warmed fluid irrigation on body temperature in arthroscopic shoulder surgery. Arthrosc: J Arthrosc Relat Surg. 2009; 25:24-29.
- Bardia A, Deshpande R, Michel G, Yanez D, Dai F, et al. Demonstration and Performance Evaluation of Two Novel Algorithms for Removing Artifacts From Automated Intraoperative Temperature Data Sets: Multicenter, Observational, Retrospective Study. JMIR Perioper Med. 2022; 5:e37174.
- Poveda VD, Nascimento AD. Controle da temperatura corporal no intraoperatório: termômetro esofágico versus termômetro timpânico. Rev Esc Enferm USP. 2016; 50:946-952.
- Putzu M, Casati A, Berti M, Pagliarini G, Fanelli G. Clinical complications, monitoring and management of perioperative mild hypothermia: anesthesiological features. Acta Bio-Med: Atenei Parm. 2007; 78:163-169.
- Kurz A. Thermal care in the perioperative period. Best Pract Res Clin Anaesthesiol. 2008;22:39-62.
- Cho S, Yoon S, Lee SJ, Jee YS, Cho CK, et al. Clinical efficacy of short-term prewarming in elderly and adult patients: A prospective observational study. Int J Med Sci. 2022; 19:1548-1556.
- Roth JV, Braitman LE, Hunt LH. Induction techniques that reduce redistribution hypothermia: a prospective, randomized, controlled, single blind effectiveness study. BMC anesthesiol. 2019; 19:1-1.
- Chun EH, Lee GY, Kim CH. Postoperative hypothermia in geriatric patients undergoing arthroscopic shoulder surgery. Anesth Pain Med. 2019;14:112-116.
- Sessler DI. Complications and treatment of mild hypothermia. J Am Soc Anesthesiol. 2001;95:531-543.
- Shin KS, Lee GY, Chun EH, Kim YJ, Kim WJ. Effect of short-term prewarming on body temperature in arthroscopic shoulder surgery. Anesth Pain Med. 2017;12:388-393.
- Shaw CA, Steelman VM, DeBerg J, Schweizer ML. Effectiveness of active and passive warming for the prevention of inadvertent hypothermia in patients receiving neuraxial anesthesia: A systematic review and meta-analysis of randomized controlled trials. J Clin Anesth. 2017; 38:93-104.
- Koh W, Chakravarthy M, Simon E, Rasiah R, Charuluxananan S, et al. Perioperative temperature management: a survey of 6 Asia–Pacific countries. BMC Anesthesiol. 2021; 21:1-0.
- Lim SH, Lee W, Park J, Kim MH, Cho K, et al. Preoperative interscalene brachial plexus block aids in perioperative temperature management during arthroscopic shoulder surgery. Korean J Anesthesiol. 2016; 69:362-367.