Research Article - Onkologia i Radioterapia ( 2022) Volume 16, Issue 10
Possibilities and limitations of left breast IMRT techniques in practice IMRT S&S versus VMAT
Rachid Errifai1*, Siham Bouaouad1 and B.K. El gueddari22Cheikh Zaïd International University Hospital, Rabat, Morocco
Rachid Errifai, Medical physics department, Cheikh Zaïd International University Hospital, Rabat,, Morocco Team of Energetics and Physics of Nuclear Reactors, Nuclear Safety and Environment, Department of Physics, Faculty of Science, Mohammed V Univ, Morocco, Email: rachiderrifai@gmail.com
Received: 13-Sep-2022, Manuscript No. OAR-22-74550; Accepted: 01-Oct-2022, Pre QC No. OAR-22-74550 (PQ); Editor assigned: 15-Sep-2022, Pre QC No. OAR-22-74550 (PQ); Reviewed: 28-Sep-2022, QC No. OAR-22-74550 (Q); Revised: 30-Sep-2022, Manuscript No. OAR-22-74550 (R); Published: 01-Oct-2022
Abstract
Introduction: The purpose of this manuscript is to compare dosimetry differences based on two types of radiotherapy plans for postoperative left breast cancer. In particular, based on a clinical dosimetric study, intensitymodulated radiation therapy (IMRT) and volumetric-modulated Arc Therapy (VMAT) plans were implemented in 10 cases of postoperative left breast cancer patients and nodes.
Material and Methods: In our study, the prescribed dose was 50 Gy to the target volume delivered in 25 fractions of 2 Gy. The dose objectives at the PTV (Planning Target Volume) and the OAR (Organs at Risk) are detailed in Table 1. The main objective was to respect a good coverage of the target volume (PTV). For the contralateral lung, contralateral breast, and heart, the objective was to achieve the lowest possible dose.
Results: For target volume coverage (PTV): Table 1 and Table 1 show that all the dosimetric criteria are met regardless of the technique. The PTV volume receiving at least 95% of the prescribed dose is lower than 95% with a major contribution of the VMAT technique compared to the S&S IMRT technique of 2.6%. The maximum dose received by the PTV is lower in VMAT than in S&S IMRT by 0.4%. For the SROs: the result is similar in both techniques, however a decrease of 1.7% of the dose received by the homolateral lung receiving at least 20 Gy is noted in favor of the S&S IMRT technique (Table 2). The dose to the heart is generally higher with VMAT, with a maximum difference of 22.2% for the heart volume receiving at least 10 Gy. Regarding treatment time, it is reduced from 11 min with S&S IMRT to 2 min with VMAT.
Conclusions: We have shown that for the treatment of breast cancer, the VMAT technique offers better dose conformation at the PTV and lower peak doses compared to S&S IMRT, For the homolateral lung, contralateral breast, and healthy tissues, VMAT allows a decrease of the doses received compared to IMRT S&S but this is accompanied by an increase of the dose received by the heart for the volume of the heart receiving at least 10 Gy, this is also accompanied by a very significant reduction of the treatment time in favor of the VMAT technique.
Keywords
Breast cancer, dosimetry, PTV, OAR, VMAT, IMRT
Introduction
Radiation therapy has become one of the vital measures in the postoperative treatment of breast cancer. It is also the most important means of improving the rate of local tumor control, as well as reducing the complication of normal tissue. The scope of radiation therapy mainly covers the chest wall and lymph nodes at positions above and below the collarbone. The technology of radiation therapy is more complex, and to avoid overlap and omission of adjacent radiation, reducing radiation damage to normal tissues without missing the target area should be considered a basic requirement for radiation therapy [1].
T he IMRT treatment technique has become a standard in many clinical locations including ORL and prostate cancers, and the use of IMRT in the particular case of breast irradiation is still widely discussed [2]. Discussions focus in particular on the longterm clinical effects.
T he use of IMRT with stationary beams has been widely discussed in the literature and many authors have demonstrated its feasibility and even its dosimetry contribution compared to nonintensity-modulated techniques. This article aims to compare the dosimetry differences based on two types of radiotherapy plans for postoperative left breast cancer. In particular, based on a clinical dosimetry study, Intensity-Modulated Radiation Therapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) plans [3, 4]. In 10 postoperative patients with left breast cancer and indication for irradiation, irradiation of the entire left mammary gland, the left Supra Clavicular (SC) area, and the left Internal Mammary Chain (IMC) was performed. The analysis focused on the evaluation of dose distributions, including the efficiency of the treatment plans. The analysis focused on the evaluation of dose distributions, including the efficiency of the treatment plans.
T his paper aimed to compare the dosimetry parameters and to obtain the most superior radiotherapy technique, i.e., to obtain the optimal dosimetry distribution of the target and to minimize the dose delivered to the lung by designing three radiotherapy plans for a certain case.
Materials and Methods
Dose description
Case selection:
The study was carried out in a random heterogeneous series of 10 patients of radiotherapy for breast cancer in our hospital in February 2017 and February 2020, treated by IMRT (Intensity Modulated Radiation Therapy (Step and Shoot (S&S)), and VMAT (Volumetric Modulated Arc Therapy), presenting carcinoma glandular breast with lymph node extension (sus clavicular) after lumpectomy, the dose prescription was 50 Gy to the target volume: PTV (Planning Target Volume) delivered in 25fractions of 2 Gy, 99% of the CTV is expected to receive at least 95% of the prescription dose (47.50Gy). The clinical constraints are as follows: VTC ≤ 107%, minimum dose ≥ 95%.
T he dose objectives at the PTV and the Organ at Risk (OAR) are detailed in (Table 1). The main objective was to achieve good coverage of the Planning Target Volume (PTV). For the contralateral lung, contralateral breast, and heart, the objective was to achieve the lowest possible dose.
Tab. 1. Dose targets defined for IMRT S&S and VMAT
| Structure name | Cost function | Threshold (gy) | Iso constraint |
|---|---|---|---|
| Ptv50 | Target penalty | 48 | |
| Quadratic overdose | 52 | 0.02 | |
| Lung left | Parallel | 5 | 60 |
| Parallel | 20 | 30 | |
| Lung right | Parallel | 5 | 6 |
| Parallel | 4 | 10 | |
| Oesophageal | Quadratic overdose | 47 | 0.08 |
| Heart | 8 | 0.08 | |
| Brest right | Parallel | 5 | 40 |
| Parallel | 25 | 10 | |
| Spinal cord | Serial | 20 | |
| Spinal cord PRV | Serial | 23 | |
| Body | Quadratic overdose | 43.5 | 0.1 |
| Body | Quadratic overdose | 40.5 | 0.6 |
Patients were positioned supine on an inclined plane with their arms raised above their heads (Figure 1). Volume delineation was performed from Computed Tomographic (CT) images with a slice thickness of 3 mm taken in the treatment position according to the RTOG (Radiation Therapy Oncology Group) contouring recommendations.
The PTV corresponds to the left breast, the supraclavicular areas, and the MIC. The PTV is defined from the CTV with a 3D margin of 5 mm limited to the external contour. The defined SROs are homolateral lung, contralateral lung, heart, and contralateral breast.
Planning dosimetry
Two processing ballistics using 6 MV X-ray photon beams delivered on an Agility gas pedal with 160 MLC were compared: an IMRT S&S type ballistic and a VMAT type ballistic [5, 6]. The TPS used is MONACO (version 5.11.02) and the Monte Carlo algorithm for S&S ballistics uses 7 beams distributed between (350°, 310°, 135°, 0°, 45°, 90°, and 180°) [7]. In VMAT 2 arcs from 300° to 240° and from 240° to 300° depending on the minimum segment size of 6 cm² and 4 MU minimum per segment.
NB
The same constraints were used for both treatment techniques. All the treatment plans in this chapter were made by the same operator.
Results
Distribution of the dose
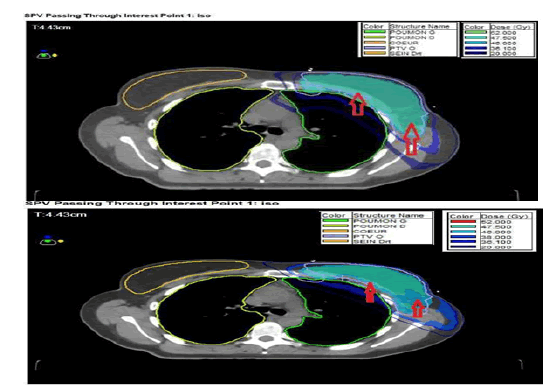
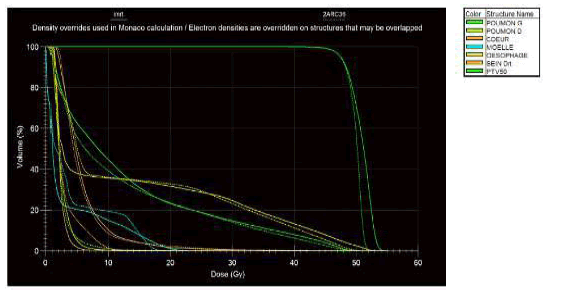
Figure 2 shows that: the VMAT technique allows a better conformation of the doses to the target volume: PTV (red arrows in the clinical case), the volume of the PTV receiving doses greater than or equal to 104% of the prescribed dose (52 Gy) is lower with VMAT than with S&S IMRT. Figure 3 represents the HDV obtained on the PTV and the main OARs. It can be seen that the two curves differ between the two techniques: the curves representing the doses received by the PTV, the heart and the contralateral breast in VMAT are above those obtained in S&S IMRT, and the curve representing the dose received by the homolateral lung is below that obtained in S&S for doses higher than 5 Gy, we also notice that the curve representing the dose received by the heart in VMAT is above that obtained in S&S IMRT and the curve representing the dose received by the contralateral lung in VMAT is below that obtained in S&S IMRT
Figure 2: Dose distribution in axial planes obtained in S&S IMRT (bottom) and VMAT (top). PTVs are shown in blue
Figure 3: HDV obtained in S&S IMRT (solid line) and VMAT (dashed line)
For the PTV, the table shows that all dosimetric criteria are respected whatever the technique and also are respected for the OAR. The volume of PTV receiving at least 95% of the prescribed dose is less than 95% with a major contribution of VMAT compared to IMRT S&S is 0.97%. The maximum dose received by PTV is lower in VMAT than in IMRT S&S by 0.4%. Regarding SROs, Table 2 shows that S&S IMRT allows a decrease in the dose received by the homolateral lung with a decrease of 1.7% for the lung volume receiving at least 20 Gy. The dose to the heart is generally higher in VMAT, with a maximum difference of 3.32% for the heart volume receiving at least 5 Gy.
Tab. 2. Dosimetric comparison between S&S and VMAT plans, values obtained on two patients for mammary gland irradiation
| Techniques | VMAT | SS | Relative gap(%) ((XVMAT- XSS)/XSS) 100 | |
|---|---|---|---|---|
| PTV 50 | PTV = (Breast left, Susclave and CMI) + 5mm | |||
| HI | 1.12 ± 0.1 | 1.06 ± 0.09 | ||
| D95 % (GY) | 46 .85 ± 1.22 | 47 .3 ± 1.97 | 0.0097 | |
| D98 % (GY) | 44 .95 ± 1.87 | 45 .85 ± 1.92 | 0.02 | |
| D2% (GY) | 53.13 ± 1.22 | 52.6 ± 1.08 | 0.01 | |
| Dmean % (Gy) | 50.83 ± 1 .6 | 59.98 ± 0.86 | 0.003 | |
| OAR Technical | Techniques | VMAT | SS | P value |
| Spinal cord | D2%(Gy) | 16 ± 1.429 | 17 ± 2.887 | 0.7967 |
| Dmean(Gy) | 19.85 ± 1.75 | 21.01 ± 2.77 | 0.9771 | |
| PRV Spinal Cord | D2 % (Gy) | 18.17 ± 1.429 | 20.6 ± 1.887 | 0.7967 |
| Dmean (Gy) | 22.85 ± 2375 | 24.01 ± 2.77 | 0.9771 | |
| Infected lung | Dmean (Gy) | 13.11 ± 3.669 | 14.62 ± 3.373 | 0.901 |
| V5 (Gy) (%) | 53.75 ±3.05 | 60.27 ± 3.08 | 0.952 | |
| V10 Gy (%) | 36.6 ± 3.553 | 42.56 ± 4.545 | 0.822 | |
| V20 Gy (%) | 22.57 ± 4.932 | 24.52 ± 4.884 | 0.715 | |
| V30 Gy (%) | 13.53 ± 2.877 | 15.72 ± 2.424 | 0.523 | |
| Contralateral lung | Dmean (Gy) | 2.11 ± 1.669 | 3.62 ± 1.373 | 0.901 |
| V5 (Gy) (%) | 3.75 ±1.05 | 2.27 ± 1.08 | 0.952 | |
| V10 Gy (%) | 1.06 ± 1.553 | 0.56 ± 0.545 | 0.822 | |
| Contralateral Breast | Dmean (Gy) | 3.11 ± 1.09 | 2.62 ± 1.03 | 0.901 |
| Heart | V5 (Gy) (%) | 33.75 ±2.05 | 36.27 ± 2.08 | 0.952 |
| V10 Gy (%) | 14.06 ± 1.553 | 12.56 ± 2.545 | 0.822 | |
| V20 Gy (%) | 7.06 ± 1.553 | 9.56 ± 2.545 | 0.622 | |
| V30 Gy (%) | 5.06 ± 1.553 | 8.56 ± 2.545 | 0.722 | |
| Dmean (Gy) | 7.06 ± 1.553 | 8.56 ± 2.545 | 0.622 | |
The efficiency of the treatment plan
Treatment time is reduced from 11 min in S&S IMRT to 2 min in VMAT.
Discussion
T he comparison made in this study suggests a better dose conformation to the PTV in VMAT technique compared to the IMRT S&S technique [8, 9]. While the dose to the OARs in the two planes was similar, the volumes in the IMRT and VMAT planes become almost similar from 150 Gy onwards, while the doses to the homolateral lung, contralateral breast, and other healthy tissues except the heart are independent of the technique used [8,10].
Concerning the study of the dose received by OARs located at a distance from the treated area (lens, gonad, and thyroid): no difference (difference less than or equal to 1 cGy) was measured between the two techniques. It is important to emphasize that the evaluation of low doses and the associated risk is very important in the case of breast cancer treatment in women who are sometimes young, given their increasingly long survival [8,10, 11].
In this study, the dose delivery time in VMAT was divided by 3.9 compared to that in IMRT S&S. Treatment times for VMAT reported in the literature range from 1.2 min to 4 min compared to 1.2 min to 3 min in our study. The limitation of treatment time is essential in the case of breast cancer treatment. Indeed, the position, on an inclined plane with the arms raised, is often uncomfortable for the patients, which can increase the risk of intra-fraction movements [12].
In addition, a major problem in the context of irradiation is the consideration of the respiratory motion. In the current practice, simple solutions have been developed for IMRT treatment by stationary beams according to two approaches: the first one consists of the inclusion in the optimization process of a virtual extension of the area to be treated beyond the skin [13], the second approach consists in a minimal angulation of the inclined plane to be able to perform CBCT (Cone Beam Computed Tomography).
Finally, to establish more generalizable results, an increase in both the number of patients and the clinical scenarios studied is essential.
Conclusion
We have shown that for the treatment of left breast cancers, the VMAT technique offers a better dose conformation at the PTV as well as lower peak doses compared to S&S IMRT. For the homolateral lung, contralateral breast, and healthy tissues, VMAT allows a decrease in the dose received compared to S&S IMRT but this is accompanied by an increase in the dose received by the heart. There is no difference between the two techniques regarding the doses received by organs outside the treatment field. We also demonstrated the potential of VMAT to limit treatment delivery time to 3 min which would allow for better treatment reproducibility. Despite this theoretical advantage of VMAT over IMRT S&S for the treatment of left breast cancer, particular attention must be paid to respect the dose objectives, in particular the coverage of the target volume whatever the technique used.
References
- Caroline Lafond. Analysis and optimization of the performance of the VMAT technique for its use in radiotherapy. Signal and image processing. HAL-Inria. 2013.
- Boxall P. Elekta VMAT: The intelligence behing VMAT. Eleta White Paper. 2011.
- Fippel M, Haryanto F, Dohm O, Nüsslin F, Kriesen S. A virtual photon energy fluence model for Monte Carlo dose calculation. Med Phys. 2003;30:301-311.
- Bedford JL, Thomas MD, Smyth G. Beam modeling and VMAT performance with the Agility 160‐leaf multileaf collimator. J Appl Clin Med Phys. 2013;14:172-185.
- Eldebawy E, Rashed Y, AlKhaldi M, Day E. A Dosimetric Comparison of Volumetric-Modulated Arc Therapy to Intensity-Modulated Radiation Therapy in the Treatment of Locally Advanced Rectal Carcinoma. Iran J Med Phys. 2020;17:374-379.
- Singh H, Gandhi A, Sapru S, Khurana R, Hadi R, et al. Comparison of Volumetric Modulated Arc Therapy and Three-Dimensional Conformal Radiotherapy in Postoperative High-Grade Glioma: A Dosimetric Comparison. Iran J Med Phys. 2019;16:385-391.
- Agility and InteriM R3.0 Clinical Mode User Guide. ELEKTA. 2012.
- Popescu CC, Olivotto IA, Beckham WA, Ansbacher W, Zavgorodni S, et al. Volumetric modulated arc therapy improves dosimetry and reduces treatment time compared to conventional intensity-modulated radiotherapy for locoregional radiotherapy of left-sided breast cancer and internal mammary nodes. Int J Radiat Oncol Biol Phys. 2010;76:287-295.
- Nicolini G, Clivio A, Fogliata A, Vanetti E, Cozzi L. Simultaneous integrated boost radiotherapy for bilateral breast: a treatment planning and dosimetric comparison for volumetric modulated arc and fixed field intensity modulated therapy. Radiat Oncol. 2009;4:1-2.
- Johansen S, Cozzi L, Olsen DR. A planning comparison of dose patterns in organs at risk and predicted risk for radiation induced malignancy in the contralateral breast following radiation therapy of primary breast using conventional, IMRT and volumetric modulated arc treatment techniques. Acta Oncol. 2009;48:495-503.
- Kikuchi K, Koyama H, Masuda H, Nomura Y, Sakai D, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival. Lancet. 2005;366:2087-2106.
- Tsai PF, Lin SM, Lee SH, Yeh CY, Huang YT, et al. The feasibility study of using multiple partial volumetric‐modulated arcs therapy in early stage left‐sided breast cancer patients. J Appl Clin Med Phys. 2012;1362-73.
- Nicolini G, Fogliata A, Clivio A, Vanetti E, Cozzi L. Planning strategies in volumetric modulated arc therapy for breast. Med Phys. 2011;38:4025-4031.