Case Report - Onkologia i Radioterapia ( 2022) Volume 16, Issue 8
Pediatric lateral retro-orbital abscess: a novel endoscopic drainage approach
Abdullah Musleh*Abdullah Musleh, Associate Professor, Consultant Otolaryngology, Head and Neck Surgery, College of Medicine, King Khalid University, Abha, Saudi Arabia, Tel: +966 56426 3377, Email: dr.abdullah.musleh@gmail.com
Received: 02-Aug-2022, Manuscript No. M-OAR-22-71048; Accepted: 22-Aug-2022, Pre QC No. M-OAR-22-71048 (PQ); Editor assigned: 04-Aug-2022, Pre QC No. M-OAR-22-71048 (PQ); Reviewed: 18-Aug-2022, QC No. M-OAR-22-71048 (Q); Revised: 20-Aug-2022, Manuscript No. M-OAR-22-71048 (R); Published: 23-Aug-2022
Abstract
A 12-year-old boy was first reported to the clinic with a complaint of a swollen right eye and impaired vision. On examination, the symptoms observed are progressive swelling, redness, photophobia, decreased vision, and restricted right eye movement. Further, the patient showed right periorbital swelling with proptosis with severe restriction on proper eye movement. Additionally, the visual acuity was significantly diminished (6/12), even though the Pupil was reactive to light. A computerized tomography (CT) scan with contrast showed a retro-orbital abscess with ring enhancement (3 cm × 2 cm), mainly towards the inferolateral aspect of the right orbit. Further, the CT scan results also revealed complete opacification of the right maxillary, anterior and posterior ethmoid paranasal sinuses. In this patient, we performed an endoscopic middle meatal antrostomy to clear the maxillary sinus in addition to Anterior and Posterior ethmoidectomies. Specifically, the lamina papyracea was partially removed to decompress the orbit and drain the pus from the orbital abscess. Using this technique, we got maximum drainage of pus, which helped to decompress the orbit and restore the vision in the patient's right eye. Also, the endoscopic drainage of pus could help the antibiotic treatment. The patient's health improved gradually with the orbit size reaching normal size and function in 5 days after antibiotic treatment. Overall, this report presents a novel endoscopic approach for draining the retro-orbital abscess, and this approach could be used to treat patients with orbital cellulitis and abscess. What makes this case unique is that in most of the cases in the literature, the endoscopic approach was successful when the abscess is localised in the medial aspect of the orbit, not in the inferolateral aspect like this case.
Keywords
Endoscopy, Impaired vision, Orbital cellulitis, Sinus, Swollen eye
Introduction
Orbital cellulitis and abscess remain the most severe complications among children [1, 2]. The common risk factors for orbital cellulitis and abscess are rhinitis and trauma, dental abscesses, intracranial and ear infections [3, 4]. Although multiple reasons could be attributed to the development of orbital cellulitis and abscess, infection by microorganisms is the most common cause [5-7]. The most common microorganisms involved in the pediatric orbital cellulitis and abscess are Staphylococcus species, Streptococcus species and Haemophilus influenza [5, 8]. Especially, orbital cellulitis caused by infections can result in devastating complications, including blindness, meningitis, intracranial abscess cavernous, cerebral venous sinus thrombosis, and subdural empyema. Even it can turn into a life-threatening condition [8-11]. Notably, out of the patients affected by orbital cellulitis, 17% died because of meningitis, and 20% of survivors lost vision permanently [12]. Therefore, early, accurate diagnosis and treatment are required in orbital cellulitis and abscess cases.
The diagnosis of orbital abscess involves a combination of clinical examination and radiographic assessment [13]. Imaging techniques like Computed Tomography (CT) of the paranasal sinuses and orbit are commonly used to assess the extent of damage and devise the treatment approach for the orbital cellulitis and abscess field [14-15]. In addition, Magnetic Resonance Imaging (MRI) is also used for assessing orbital abscesses [16]. Primarily, the orbital cellulitis and abscess are managed by administering intravenous antibiotics [13] and by the draining of the abscess by the endoscopy assisted surgery [17, 18].
In this case report, we describe a novel endoscopic drainage approach for treating paediatric lateral retro-orbital abscess diagnosed in a 12-year-old boy. We could successfully drain the abscess using a Right Endoscopic Orbital Decompression with functional Endoscopic Sinus Surgery, and the patient got discharged on the 5th day with complete recovery.
Case Report
A 12-year-old boy was first reported to the department of ophthalmology with a complaint of a swollen, painful right eye with impaired vision. Subsequently, he was transferred to the department of Otolaryngology for subsequent examination. The patient's general condition was poor, with severe pain, disturbed sleep, and diminished appetite. The patient had no previous history of nasal discharge, nasal obstruction, post-nasal drip, epistaxis or allergy. In addition, there are no otolaryngology symptoms. The patient had no prior history of surgical or medical treatment. Currently, the patient is under medication with oral broad-spectrum antibiotics. The patient seems to be febrile (100°F) with a respiratory rate of 30 per min and a heart rate of 80 per min. The symptoms observed are progressive swelling, redness, photophobia, decreased vision, and restricted proper eye movement. On eye examination, the patient was found to have the right periorbital swelling with severe Proptosis of the Right eye with strict restriction on eye movement (Figure 1).

Figure 1: Patient showing pre-operative right eye proptosis
Additionally, the visual acuity was significantly diminished (6/12). However, the Pupil was reactive to light. The basic blood parameters were found normal. However, a CT scan with contrast showed a retro-orbital abscess with ring enhancement 3 cm × 2 cm, mainly towards the inferolateral aspect of the right orbit (Figure 2). CT scan also showed complete opacification of the right maxillary, anterior and posterior ethmoid paranasal sinuses (Figure 3). Emergency surgery for draining the abscess was planned after a diagnosis of the retro-orbital abscess. Right Endoscopic Orbital Decompression with functional endoscopic sinus surgery was scheduled for the patient. An endoscopic middle meatal antrostomy was performed to clear the maxillary sinus in addition to anterior and posterior ethmoidectomies.
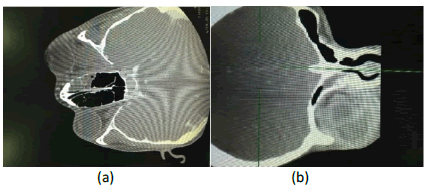
Figure 2: CT scan images showing the retro-orbital abscess with ring enhancement mainly towards the inferolateral side of the right orbit (a) Axial view of the CT scan (b) Coronal view of the CT scan
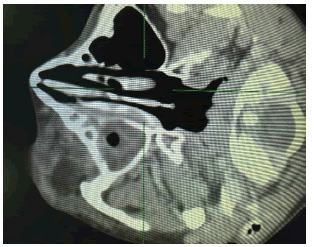
Figure 3: CT scan image showing complete opacification of the right maxillary, anterior and posterior ethmoid paranasal sinuses
The lamina papyracea was partially removed to decompress the orbit, and a large amount of pus was drained. A sample of the pus was sent for culture and antibiotic sensitivity tests. Post operatively, the patient was treated with intravenous infusions of Vancomycin and Meropenem. The patient's health improved gradually, with the orbit size reaching normal size and function in 5 days. A CT Scan was performed on the 5th day, which showed improvement and clearance of the retro-orbital abscess and the paranasal sinuses (Figure 4).
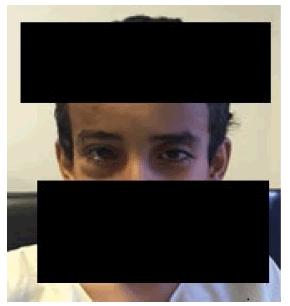
Figure 4: Patient recovered after 5th day of the surgical and medical treatment
The patient was discharged on the 5th day with a complete eye movement, normal vision (6/6) and pupil reaction (Figure 5).
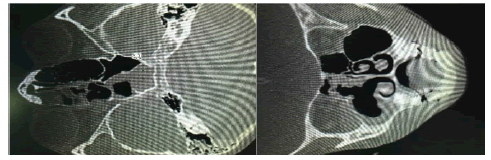
Figure 5: CT Scan images showing improvement and clearance of the retroorbital abscess and the involved paranasal sinuses
Discussion
Orbital cellulitis and abscess are primarily observed in young children but can occur in all age groups [13-15]. Of the children with orbital cellulitis, 62% were older than five years of age; Reports suggest that the incidence has a gender bias and males are prone to orbital cellulitis twice as frequently as females [19- 21]. However, another study suggests no significant difference in the susceptibility between males and females to orbital cellulitis [22]. In the present case report, the patient was a 12-yearold male. The cause of the orbital cellulitis in the patient was not known, and specifically, the patient has no history of the respiratory tract or otolaryngology symptoms. There are no signs of nasal discharge, nasal obstruction or rhinitis in the patient. Moreover, the patient has not undergone any surgery or previous history of dental abscesses, ear infections or cranial infections. These observations are interesting as most cases of orbital cellulitis are associated with predisposing factors such as upper respiratory infection, trauma to the eyelids, sinusitis and dental abscess [3, 4]. However, we cannot rule out the possibility that the infection may be subclinical and might enter the eyes through the systemic circulation. Since the patient completely recovered from the orbital cellulitis after treatment with intravenous antibiotics Vancomycin and Meropenem, we know that the patient might have acquired bacterial infections, which might be the primary cause of the orbital abscess.
Multiple risk factors have been identified for orbital cellulitis in the pediatric population. However, there are no established guidelines are reported in the previous studies. Mostly, the management is specific to the patient and the degree of disease progression. The most common organisms involved in the pathogenesis of orbital cellulitis are Streptococcus anginosus group, Group A Streptococci, Streptococcus pneumoniae and Staphylococcus aureus. In addition, the Methicillin-Resistant Staphylococcus Aureus (MRSA) was also a key concern for Orbital cellulitis [23]. Notably, MRSA positivity was observed in almost 6.5% of orbital and sinus cultures grown from orbital cellulitis patients [24].
Furthermore, the data suggest that in cultures isolated from old patients, multiple groups of organisms grew, especially anaerobic microorganisms, the most common bacteria in these samples, followed by streptococci [25]. Besides, Haemophilus influenza was also found in the cases of orbital cellulitis [26]. In another work, the most frequently identified microorganisms in patients with orbital cellulitis were S. pneumoniae, S. pyogenes and H. influenza [27]. These findings suggest that the Streptococcus species are the most common bacteria found in children with orbital cellulitis. Primarily, anaerobic bacteria are located in the cultures of orbital cellulitis patients [28]. We have not identified the microorganisms involved in this report, though we performed antibiotic sensitivity assays.
Clinically, most orbital cellulitis patients presented with swelling, redness, eyelid oedema, proptosis, and orbital pain. Also, in severe cases, the patients exhibited reduced ocular mobility and impaired visual activity [13]. In our case, we also observed similar symptoms in the patient. Studies indicate that unattended orbital cellulitis and abscess cases may end in impaired or loss of vision caused by optic neuritis, increased Intra Orbital Pressure (IOP), retinal artery thrombosis, or traction on the optic nerve [29]. Notably, in most cases, after the surgical and medical decompression, the impaired visual acuity is reversed to a certain degree even though there are no prognostic markers for predicting the reversion of vision. However, the chronic orbital cellulitis and abscess cases end in loss of vision and the possibility of lost vision; it is a very slim chance that the patient will recover his vision [30]. In our case presented in this report, we could rescue the temporary vision impairment. The patient vision was fully restored after successful right endoscopic orbital decompression with functional endoscopic sinus surgery.
Timely diagnosis is of paramount importance in treating orbital cellulitis and abscess. Medical imaging provides critical information regarding the orbital abnormalities, including orbital cellulitis and abscess. Currently, available imaging techniques provide valuable information regarding infections, vascular abnormalities, inflammation, oedema and retinal and choroidal detachments. In most eye diseases, the diagnosis is mainly performed by CT, the most useful imaging technique for diagnosing orbital cellulitis and abscesses. CT scan allows differentiation of pathological conditions like infections, inflammation and abscess to distinguish from post-therapeutic changes and physiologic changes, including calcifications [13]. A high-resolution CT is useful in imaging the eye and retroorbital tissues, intracranial sinuses, intracranial abscess or oedema, and intracranial contents. Specifically, the supra-orbital abscess appears on CT as a low-density mass, with or without ring enhancement. Further, the displacement of the globe by abscess and proptosis can be observed in addition to the spot. Additionally, an orbital abscess can be easily identified in the face of very low density and having a gas shadow in the cavity of the abscess [14, 31]. Studies indicate that the axial CT is best for identifying medial subperiosteal orbital abscess and its related intracranial complications, and coronal imaging is ideal for imaging superior or inferior orbital abscess [13, 14, 23, 31]. CT findings are instrumental in combining with the clinical findings to determine the course of treatment for patients with ocular abscesses. In addition to the CT, MRI is also a valuable imaging tool for diagnosing orbital cellulitis and abscesses and their associated intracranial complications. In MRI, orbital abscesses show a phenomenon of diffusion restriction, mostly related to the viscosity of the pus and dense cellular content found in the purulent material [13]. In this report, we used CT to diagnose the retro-orbital abscess appropriately. Both pre and post-CT scan images demonstrate the resolution of orbital abscess five days post-surgical draining.
The exact timing of medical and surgical intervention for an orbital abscess is critical to managing orbital cellulitis. Studies conducted earlier suggest that the smaller abscesses in younger children are suitable for medical treatment in a close observation by a physician [13]. Notably, the response to medical therapy is better in younger children than in older patients, and thus, they may recover faster if they have smaller abscesses [32]. The critical parameters associated with successful nonsurgical medical management of ocular cellulitis and small abscess include the patients with normal vision, minimal or no proptosis, absence of ophthalmoplegia, and medial location of the abscess [15, 27, 33]. In contrast, the larger abscess requires immediate surgical intervention to drain the puss from the large orbital abscess and obtain samples for cultures. Surgical drainage helps relieve the orbital pressure, prevent the optic nerve damage, and preserve the vision of the patient [15, 27, 33]. Clinicians choose emergency surgery if they see signs such as loss of visual acuity, nonimproving abscess, inability to perform a reliable ophthalmologic examination, and clinical deterioration of the patient even after the antibiotic treatment. In specific cases, surgical intervention is required to prevent the spread of infection to the brain [34]. Of note, the results of eight retrospective studies and case reports suggest that pediatric patients who had orbital abscesses required surgical drainage and medical management [2, 23] similar to the current case report.
Recently, the most preferred surgical intervention for decompaction is endoscopic drainage of orbital abscess, which has fewer complications and is superior to the conventional surgical techniques. The endoscopic approach involves surgical ethmoidectomy, and for the drainage of the orbital abscess, lamina papyracea was partially removed with a sickle knife or Cottleelevator [17, 35-37]. In this case, we performed an endoscopic middle meatal antrostomy to clear the maxillary sinus in addition to anterior and posterior ethmoidectomies. Specifically, the lamina papyracea was partially removed to decompress the orbit and drain the pus from the orbital abscess. Which helped soften the rotation and restore the patient's right eye vision. Also, the drainage of pus could help the antibiotic treatment, which could be the reason for the accelerated recovery of the patient. Overall, this report presents a novel endoscopic approach for draining the retro-orbital abscess, and this approach could be used to treat patients with orbital cellulitis and abscess.
Conclusion
A 12-year-old boy was first reported to the clinic with a complaint of a swollen right eye and impaired vision. On examination, the symptoms observed are progressive swelling, redness, photophobia, decreased vision, and restricted right eye movement. The patient showed right periorbital swelling with proptosis with severe restriction on proper eye movement. Additionally, the visual acuity was significantly diminished (6/12), even though the Pupil was reactive to light. A Computerized Tomography (CT) scan with contrast showed a retro-orbital abscess with ring enhancement (3 cm × 2 cm), mainly towards the inferolateral aspect of the right orbit. Then CT scan results also revealed complete opacification of the right maxillary, anterior and posterior ethmoid paranasal sinuses. In this patient, we performed an endoscopic middle meatal antrostomy to clear the maxillary sinus in addition to Anterior and Posterior ethmoidectomies. Specifically, the lamina papyracea was partially removed to decompress the orbit and drain the pus from the orbital abscess. Using this technique, we got maximum drainage of pus, which helped to decompress the orbit and restore the vision in the patient's right eye. Also, the endoscopic drainage of pus could help the antibiotic treatment. The patient's health improved gradually with the orbit size reaching normal size and function in 5 days after antibiotic treatment. Overall, this report presents a novel endoscopic approach for draining the retro-orbital abscess, and this approach could be used to treat patients with orbital cellulitis and abscess. The uniqueness of this case is that in most of the cases in the literature, the endoscopic approach was successful when the abscess is localised in the medial aspect of the orbit, not in the inferolateral aspect like this case.
References
- Mourouzis SN. Pediatric management problems: orbital cellulitis. Pediatr. Nurs. 1996; 22:52-53.
- Wong SJ, Levi J. Management of pediatric orbital cellulitis: a systematic review. Int. J PediatrOtorhinolaryngol. 2018; 110:123-129.
- Tariq Farooq B, Mir Z, Mohammad Naeem K, Mohammad Daud K. Risk factors of preseptal and orbital cellulitis.[Google Scholar]
- Janakarajah N, Sukumaran K. Orbital cellulitis of dental origin: case report and review of the literature.Br J Oral Maxillofac Surg. 1985;23:140-145.
- McKinley SH, Yen MT, Miller AM, Yen KG. Microbiology of pediatric orbital cellulitis. Am Jophthalmol, 2007;144:497-501.
- Gonzalez MO, Durairaj VD. Understanding pediatric bacterial preseptal and orbital cellulitis. Middle East Afr J Ophthalmol,2010;17:134.
- Meyer DR, Nagi K. Allergic fungal sinusitis with subperiosteal orbital abscess. Arch Ophthalmol.2005;123:1281-1282.
- Hsu J, Treister AD, RalayRanaivo H, Rowley AH, Rahmani B. Microbiology of pediatric orbital cellulitis and trends in methicillin-resistant Staphylococcus aureus cases.ClinPediatr.2019;58:1056-1062.
- Todman MS, Enzer YR. Medical management versus surgical intervention of pediatric orbital cellulitis: the importance of subperiosteal abscess volume as a new criterion.Ophthalmic PlastReconstr Surg. 2011; 27:255-259.
- Reynolds DJ, Kodsi SR, Rubin SE, Rodgers IR. Intracranial infection associated with preseptal and orbital cellulitis in the pediatric patient. J Am AssocPediatrOphthalmol Strabismus. 2003; 7:413-417.
- Zhinkova NM. Orbital abscess and brain abscess as complications of purulent frontitis and ethmoiditis. Vestn Otorinolaringol.1976; 6:76-77.
- Satar HA, Yaakub A, Shukri NM, Tajudin LS. Orbital Cellulitis Secondary to Dental Abscess in Children. Cureus. 2021;13.
- Bedwell J, Bauman NM. Management of pediatric orbital cellulitis and abscess. Curr Opin Otolaryngol Head Neck Surg. 2011;19:467-473.
- Cherry JR. CT scanning in orbital cellulitis.J R Soc Med. 1988;81:124.
- Sciarretta V, Demattè M, Farneti P, Fornaciari M, Corsini I, et al. Management of orbital cellulitis and subperiosteal orbital abscess in pediatric patients: a ten-year review. Int J Pediatr Otorhinolaryngol. 2017; 96:72-76.
- Jain SF, Ishihara R, Wheelock L, Love T, Wang J, et al. Feasibility of rapid magnetic resonance imaging (rMRI) for the emergency evaluation of suspected pediatric orbital cellulitis. J Am AssocPediatrOphthalmol Strabismus. 2020; 24:289-e1.
- Manning SC. Endoscopic management of medial subperiosteal orbital abscess. Arch Otolaryngol–Head Neck Surg. 1993;119:789-791.
- Bhargava D, Sankhla D, Ganesan A, Chand P. Endoscopic sinus surgery for orbital subperiosteal abscess secondary to sinusitis. Rhinology. 2001;39:151-155.
- Nageswaran S, Woods CR, Benjamin Jr DK, Givner LB, Shetty AK. Orbital cellulitis in children. Pediatr Infect Dis J2006; 25:695-699.
- Bazilevs Y, Hsu MC, Zhang Y, Wang W, Liang X, et al. A fully-coupled fluid-structure interaction simulation of cerebral aneurysms. Comput mech. 2010; 46:3-16.
- Georgakopoulos CD, Eliopoulou MI, Stasinos S, Exarchou A, Pharmakakis N, et al. Periorbital and orbital cellulitis: a 10-year review of hospitalized children. Eur J Ophthalmol. 2010; 20:1066-1072.
- Fearon B, Edmonds B, Bird R. Orbital-facial complications of sinusitis in children. Laryngoscope. 1979; 89:947-953.
- Burek AG, Melamed S, Liljestrom T, Qi J, Kelly TG, et al. Evaluation and medical management of the pediatric patient with orbital cellulitis/abscess: A systematic review. J Hosp Med. 2021; 16:680-7.
- Liao S, Durand ML, Cunningham MJ. Sinogenic orbital and subperiosteal abscesses: microbiology and methicillin-resistant Staphylococcus aureus incidence. Otolaryngol-Head Neck Surg. 2010; 143:392-396.
[Google Scholar] [Cross Ref]
- Brown CL, Graham SM, Griffin MC, Smith RJ, Carter KD, et al. Pediatric medial subperiosteal orbital abscess: medical management where possible. Am J Rhinol. 2004; 18:321-327.
- Londer L, Nelson DL. Orbital cellulitis due to Haemophilus influenzae. Arch Ophthalmol. 1974; 91:89-91.
- Ikeda K, Oshima T, Suzuki H, Kikuchi T, Suzuki M, et al. Surgical treatment of subperiosteal abscess of the orbit: Sendai's ten-year experience. Auris Nasus Larynx. 2003;30: 259-62.
- Ketenci I, Ünlü Y, Vural A, Doğan H, Şahin Mİ, et al. Approaches to subperiosteal orbital abscesses. Eur Arch Oto Rhino Laryngol. 2013;270: 1317-1327.
- Schramm Jr VL, Curtin HD, Kennerdell JS. Evaluation of orbital cellulitis and results of treatment. Laryngoscope. 1982; 92:732-738.
- Giannoni CM, Stewart MG, Alford EL. Intracranial complications of sinusitis. Laryngoscope. 1997;107: 863-867.
- Roberts C, Nylander AE, Jayaramachandran S. Orbital cellulitis complicating isolated unilateral sphenoidal sinusitis: importance of the CT scan. Br J Ophthalmol.1989; 73:769-770.
- Shifman NT, Krause I, Dotan G, Gilony D, Bilavsky E. Orbital Cellulitis in a Pediatric Population-Experience From a Tertiary Center. Indian Pediatr. 2022; 59:35-37.
- Chorney SR, Buzi A, Rizzi MD. The role of endoscopic sinus surgery in children undergoing external drainage of non-medial subperiosteal orbital abscess. Am J Rhinol Allergy. 2021;35: 288-295.
- Arjmand EM, Lusk RP, Muntz HR. Pediatric sinusitis and subperiosteal orbital abscess formation: diagnosis and treatment. Otolaryngol-Head Neck Surg. 1993;109:886-894.
- Fakhri S, Pereira K. Endoscopic management of orbital abscesses. Otolaryngol Clin N Am. 2006;39: 1037-1047.
- Migirov L, Yakirevitch A, Bedrin L, Wolf M. Endoscopic sinus surgery for medial orbital subperiosteal abscess in children. J. Otolaryngol.-Head Neck Surg.2009;38.
- Page EL, Wiatrak BJ. Endoscopic vs external drainage of orbital subperiosteal abscess. Arch Otolaryngol-Head Neck Surg. 1996; 122:737-740.



