Research Article - Onkologia i Radioterapia ( 2024) Volume 19, Issue 2
Optimizing Helicobacter pylori diagnosis in oncology for enhanced radiotherapy outcomes
Shier Ali Khorsheed*Shier Ali Khorsheed, Department of Oncology, College of Science, University of Kirkuk, Kirkuk, Iraq, Email: shler-ali@uokirkuk.edu.iq
Received: 06-Oct-2023, Manuscript No. OAR-23-115912; , Pre QC No. OAR-23-115912 (PQ); Editor assigned: 09-Oct-2023, Pre QC No. OAR-23-115912 (PQ); Reviewed: 23-Oct-2023, QC No. OAR-23-115912; Revised: 11-Oct-2024, Manuscript No. OAR-23-115912 (R0; Published: 18-Oct-2024
Abstract
Helicobacter pylori consider a globally common infection, and closely related to the occurrence of stomach cancers. Since accurate diagnosis is a key factor in eradicating this infection, so this study aimed to conduct a comparison between the serology with the stool analyses for the identification of this infection. Sixty patients with dyspepsia and sixty others participated as controls in this comparative study, no statistical variation was noted between the groups in terms of gender and age. Samples required for serology (IgM) and Stool Antigen Test (SAT) were collected. The results confirmed that the prevalence of infection among all participants 120 was 61.7% and 70.0% depending on serology and SAT methods, respectively. Patients were more positive towards SAT 41.7%, compared to the controls 28.3% with a considerable difference p=0.003. Likewise for serology test, where 37.5% of the patients compared to 25.8% of the controls were positive (p=0.001). It was concluded that both serology and SAT tests of Helicobacter pylori are useful in the diagnosis of infection, and are somewhat comparable in their ability to detect infection especially in suspected endemic areas.
Keywords
Helicobacter pylori diagnosis; Helicobacter pylori pathogen; Helicobacter pylori; Serological test; Stool test; Stomach cancers; Oncology; Radiotherapy
Introduction
Almost half of the world's inhabitants are infected with Helicobacter pylori, a chronic bacterial disease caused by highly mobile, spiralshaped, or curved gram-negative bacteria with multiple flagella that selectively colonize the gastric epithelium Helicobacter pylori IgM test is a blood analysis used to detect the presence of IgM antibodies for stomach germ, which indicates the presence of an individual with stomach germ. The stomach germ or the infection of the gastrointestinal infection is one of the infections that affects the digestive system, which may cause digestive disorder such as gastritis, or digestive ulcers, and in some medical cases it leads to stomach cancer, and it is worth noting that [1-3]. The majority of individuals infected with this bacteria may remain asymptomatic throughout their lives, and according to documented genetic studies, this organism was settled in the stomach of humans very decades ago and evolved with humans over time [4,5]. In nondeveloped countries, the prevalence rate is high due to poor health as well as social and economic living conditions compared to developed countries [6,7].
As for Iraq, according to a few studies, the prevalence of H. pylori infection ranges from (11%-71%), despite the lack of accurate statistics and information on that [8]. A variety of gastrointestinal diseases are associated with this infection, including ulcers of the stomach and small intestine [9], even though most individuals with stomach germs do not have symptoms, but stomach germ reduces the ability of the stomach to produce mucus, which makes the stomach vulnerable to damage due to the acid in it. It has been considered a class I carcinogen for stomach cancer, this bacteria is the main causative agent of infection-related cancers, which represents five percent of global cancer around the world [10,11].
For this reason, it is very important to diagnose this infection, which contributes to monitoring the effectiveness of the treatment to eliminate it [12]. Invasive and non-invasive analyses contribute mainly to the diagnosis of H. pylori infection, and the choice of technique is based on the case of each patient [13]. In general, the diagnosis of infection with this organism begins with noninvasive testing methods, in which serology, as well as stool antigen assessments, are the most commonly used. These non-invasive analyses are preferred in certain cases, and each of them has specific characteristics [14,15]. Although these assessments are unable to detect complications associated with infection, they nonetheless remain a desirable evaluation due to their ease of use and providing results within a few minutes [16]. The present study aimed to compare the serological method with antigen testing for H. pylori infection diagnosis. Stool antigen tests performed via immunoassay can determine H. pylori infection in a large number of subjects and can be used for serologic diagnosis of the infection. In Japan, a stool antigen test, which uses monoclonal antibody to H. pylori native catalase was developed and use of this test, becoming popular in the diagnosis of H. pylori infection [17]. Stool antigen tests are also a type of non-invasive tests for diagnosing H. pylori infection. Recently, several stool antigen tests, which use monoclonal antibodies, have been established [18]. Survey as well as serology. However, previous studies examined the diagnostic usefulness of stool antigen test in patients with gastroduodenal diseases and no study has examined the applicability of stool antigen tests to determine H. pylori infection in healthy adult subjects who receive mass survey. In this study, to clarify if a stool antigen test is worth to perform in a mass survey instead of serology, we examined H. pylori infection by both serology and a stool antigen test in a mass survey in order to evaluate the differences of both tests for screening of H. pylori infection and to study the factors that might cause discrepancies between the results obtained by the two test [19].
Materials and Methods
Out of a total of 120 participants in this comparative study 60 of them were suffering from gastrointestinal disorders, especially dyspepsia, and 60 others were healthy (for control) who attended Azadi teaching hospital and some private clinics in Kirkuk Governorate, northern Iraq, during the period from April 2021 until March 2022. This study was conducted after obtaining the fundamental approvals followed by the local ethical committee of the health directorate. This study included both genders, aged eighteen years and over, after obtaining informed consent to participate in the study. The control participants had no history of gastrointestinal disease. As for the patient’s participants, the inclusion criteria were the persistence of dyspeptic symptoms for period of at least three months. Exclusion criteria included pregnant, patients with critical liver and kidney problems, also who received the following: Antibiotics, proton pump inhibitors, and H2 receptor blockers at least one month prior to the study. Stool samples as well as serum samples were collected from these participants and kept at -20°C until use. Both methods (serological and stool tests) were evaluated in all patients. Using an enzyme immunoassay kit (HpSA) TM, stool samples were analyzed for the antigen of each participant based on the manufacturer's instructions. Whereas, sera were analyzed for IgM antibodies using a commercial Premier EIA kit (HpIgM). After data acquisition and collection, IBM (SPSS) statistics version 26 program was used to analyze the results, which were tabulated and expressed in frequencies and percentages. Comparison between the two groups (patients and controls) was made using chi-square with the P-value considered considerable at less than 5 percent.
Results
Around 60 participants (patients) with dyspepsia symptoms and 60 other participants (control), this study was conducted (Table 1).
| Characteristics | Controls N=60 50% |
Patients N=60 50% |
Total N=120 100% | P-value | |
|---|---|---|---|---|---|
| Gender | Male | 33 (27.5%) | 36 (30%) | 69 (52.7%) | 0. 96 |
| Female | 23 (22.5%) | 24 (20.0%) | 47 (47.5%) | ||
| Age | 21-30 | 4 (3.3%) | 9 (7.5%) | 13 (10.8%) | 0.37 |
| 31-40 | 18 (15.0%) | 19 (15.8%) | 37 (32.5%) | ||
| 41-50 | 19 (15.8%) | 25 (20.8%) | 44 (36.7%) | ||
| 51-60 | 11 (9.2%) | 13 (10.8%) | 24 (20%) | ||
Tab. 1. The baseline characteristics of the individuals participating (N=120).
It shows that males are more injured than females where the results appeared as patients 36 (30.0%) and the control 33 (27.5%) the total was 69 (52.5%). As for the proportions of the females, such as the control 24 (20.0%) and the patients 23 (22.5%) and the total 47 (47.5%) if through comparison you are the percentage of the injured males are the most numerous, while the females are the least infected in the control and patient test. As for the age group, it was like the ages of the age group (21-30), they were the least injury, as the proportions were such as the patients (7.5%) 9 and the control 4 (3.3%) the total 13 (10.8%) and the age group is followed in the lack of injury (51-60) The proportions were like patients with patients 13 (10.8%) and the control 11 (9.2%) the total number is 24 (20.0%). Then it is followed by the age group (31-40) the proportions were like patients with patients 19 (15.8%) and the control is 18 (15.0%) the total number 37 (32.5%). Then it is followed by the age (41-50). The percentage of patients was 25 (20.8%), while the control was 21 (17.5%) the total number was 46 (36.7%).
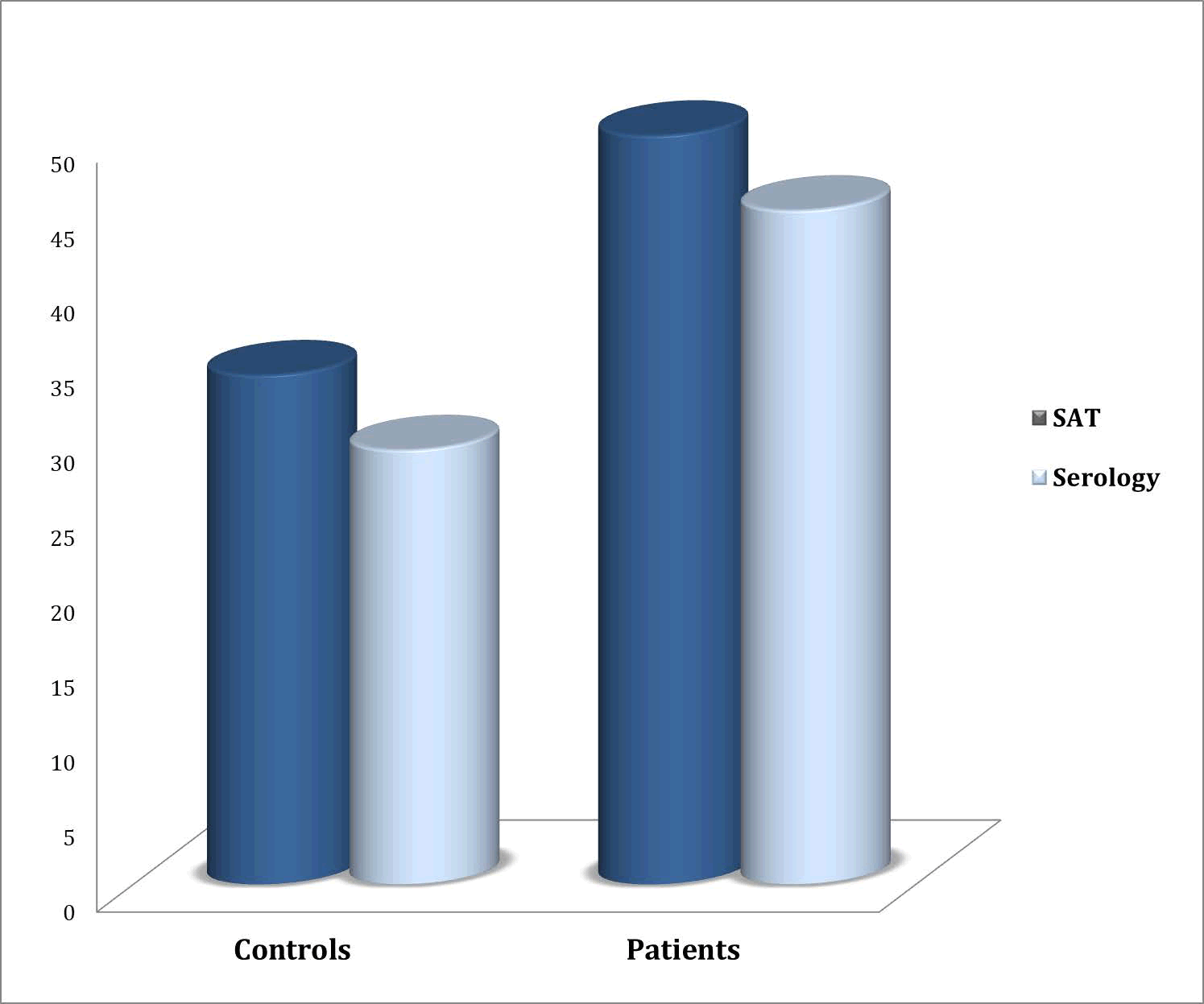
After conducting both diagnostic tests for H. pylori infection, Stool Antigen Test (SAT) and serology, the preliminary results indicated that the incidence of H. pylori infection was more in patients compared with the control group as shown in Figure 1.
For the Stool Antigen Test (SAT), 50 (41.7%) of the dyspepsia patients were positive compared to 34 (28.3%) among the controls (p=0.003). As for the serological test (IgM), the results were also more positive in the patients 45 (37.5%) compared to the controls 31 (25.8%), versus with statistical significance (p=0.001) as illustrate in Table 2.
Fig. 1. Incidence of Helicobacter pylori infection among participants using the diagnosed methods.
| Tests | Patients N=60 50% |
Controls N=60 50% |
Total N=120 100% | P value | |
|---|---|---|---|---|---|
| SAT | Positive | 50 (41.7%) | 34 (28.3%) | 84 (70%) | 0.003 |
| Negative | 10 (8.3%) | 16 (21.7%) | 26 (10.7%) | ||
| Serology | Positive | 45 (37.5%) | 31 (25.8%) | 76 (61.7%) | 0.001 |
| Negative | 15 (12.5%) | 14 (24.2%) | 29 (38.3%) |
Tab. 2. Comparison of positive results SAT versus serology tests among participants.
Serology tests if: The result is negative if it is less than 30 milligrams/ dl. The possibility of infection increases if the result ranges between 30.01-39.99 milligrams/ dl. The result is positive if it is more than or equal to 40 milligrams/ dl.
Discussion
There are tests for Helicobacter pylori whose results are given in the form of a ratio such as the analysis of stomach bacteria in the blood. Helicobacter pylori blood analysis reveals the presence of antibodies; they are proteins made by the immune system in response to bacteria, such as IgM and IgG, and their levels are measured in the blood as well as through stool test. It was found that the ratio of females to males is less infected with Helicobacter pylori infection. As for the most affected age group, they are between (41-50), which is the age group that works, that is, the producer may stay for a long time without eating or eating foods outside the home or rely on a lack of immunity or genetic factor, so the positive infections were males in our study compared to females.
Diagnostic screening for Helicobacter pylori infection is often recommended for people with gastrointestinal disorders, including dyspepsia [17,18]. Several diagnostic methods have been developed, which are divided into possible blood antibody tests, Urea breath tests, stool antigen tests, stomach biopsy, or endoscopic methods, according to the requirements of each case [19]. Non-invasive diagnostic tests are preferred as the first choice because they are convenient and do not require an endoscopic procedure, in addition to their low cost. The Stool Antigen Test (SAT) is an important method in diagnosing infection with Helicobacter pylori infection, as it has many advantages, including ease of implementation, and is not affected by drugs, and it may also be used in following up infected patients after treatment, as it reveals the presence of active infection, is relatively inexpensive and easy to obtain on the sample. Besides, this test can be easily used in pregnancies as well as at all ages and does not require a very complicated laboratory facility. When using the SAT test, the incidence of Helicobacter pylori infection was detected at a rate of 70.0%. Our finding was in agreement with the recent validation study conducted to detect Helicobacter pylori infection in Iraqi patients with gastrointestinal problems and found that the incidence of H. pylori in Iraqi patients, it ranged between 50 (41.7%), while the control ratio was 34 (28.3%), if the scores were positive for the SAT, while the negative results were less than 30, as shown in Table 2. As for the serological examination, 45 (37.5%) were positive because they are more of the 40 and control 31 (25.8%) are at risk of Helicobacter pylori infection. They showed that successful treatment of gastrointestinal problems depends mainly on an accurate diagnosis of Helicobacter pylori in the early stages of infection, and they emphasised the use of a combination of non-invasive and invasive methods to diagnose infection, including SAT, and to obtain an accurate analysis. Diagnosis is the best option for initial treatment. As for the serological method, one of its drawbacks is the inability to distinguish between current and previous infections, and this may explain the poor accuracy of serological analyses in general [20].
Although the positive results in the current study amounted to 61.7%. In a similar study conducted in Ethiopia on 201 dyspepsia patients, they concluded that the SAT test was superior to the serology test and recommended that the SAT could be used to identify (active) Helicobacter pylori infection before starting treatment among dyspepsia patients.
Conclusion
Serological test help diagnose an individual with a portal infection or verify that treatments used to treat a portal infection are effective and successful in treatment, or check the symptoms an individual is experiencing in the gastrointestinal tract due to Helicobacter pylori.
It is concluded that serum IgM of both Helicobacter pylori and SAT are both useful in diagnosing infection and are somewhat comparable in their ability to detect infection, even in highly endemic areas. The SAT test was superior to the serology test and it was recommended to use the SAT test to determine active Helicobacter pylori infection before starting treatment among dyspepsia patients because the serological method may remain the antibodies in the blood for a longer period even after treatment so the SAT test is recommended although it has some drawbacks as the time between obtaining and analysing the stool and the temperature surrounding the sample are all factors that have a role in changing the sample and the result, but it is the best.
References
- Rostami H, Haddadi MH. Benzimidazole derivatives: A versatile scaffold for drug development against Helicobacter pylori-related diseases. Fundam Clin Pharmacol. 2022; 36:930-943.
[Crossref] [Google Scholar] [PubMed]
- Awuku YA, Simpong DL, Alhassan IK, Tuoyire DA, Afaa T, et al. Prevalence of Helicobacter pylori infection among children living in a rural setting in Sub-Saharan Africa. BMC Public Health. 2017; 17:1-6.
[Crossref] [Google Scholar] [PubMed]
- Yadav AK, Verma D, Chaudhary N, Kumar A, Solanki PR. Aptamer based switches: A futuristic approach for Helicobacter pylori detection. Mater Lett. 2022; 308:131239.
- Stefano K, Marco M, Federica G, Laura B, Barbara B, et al. Helicobacter pylori, transmission routes and recurrence of infection: state of the art. Acta Biomed. 2018; 89:72-76.
[Crossref] [Google Scholar] [PubMed]
- Waskito LA, Yamaoka Y. The story of Helicobacter pylori: Depicting human migrations from the phylogeography. Helicobacter pylori in human diseases. Adv Microbiol Infect Dis Public Health. 2019; 11:1-6.
[Crossref] [Google Scholar] [PubMed]
- Bagirova M, Allahverdiyev AM, Abamor ES, Aliyeva H, Unal G, et al. An overview of challenges to eradication of Helicobacter pylori infection and future prospects. Eur Rev Med Pharmacol Sci. 2017; 21:2199-2219.
[Google Scholar] [PubMed]
- Cano-Contreras AD, Rascon O, Amieva-Balmori M, Rios-Galvez S, Maza YJ, et al. Approach, attitudes, and knowledge of general practitioners in relation to Helicobacter pylori is inadequate. There is much room for improvement. Rev Gastroenterol Mex. 2018; 83:16
[Crossref] [Google Scholar] [PubMed]
- Karkhah A, Ebrahimpour S, Rostamtabar M, Koppolu V, Darvish S, et al. Helicobacter pylori evasion strategies of the host innate and adaptive immune responses to survive and develop gastrointestinal diseases. Adv Microbiol. 2019; 218:49-57.
[Crossref] [Google Scholar] [PubMed]
- Hussein RA, Al-Ouqaili MT, Majeed YH. Detection of Helicobacter pylori infection by invasive and non-invasive techniques in patients with gastrointestinal diseases from Iraq: A validation study. Plos One. 2021; 16:e0256393.
[Crossref] [Google Scholar] [PubMed]
- Moss SF. The clinical evidence linking Helicobacter pylori to gastric cancer. Cell Mol Gastroenterol Hepatol. 2017; 3:183-191.
[Crossref] [Google Scholar] [PubMed]
- Ishaq S, Nunn L. Helicobacter pylori and gastric cancer: A state of the art review. Gastroenterol Hepatol. 2015; 8:S6.
[Google Scholar] [PubMed]
- Lee YC, Dore MP, Graham DY. Diagnosis and treatment of Helicobacter pylori infection. Annu Rev Med. 2022; 73:183-195.
[Crossref] [Google Scholar] [PubMed]
- Sabbagh P, Mohammadnia-Afrouzi M, Javanian M, Babazadeh A, Koppolu V, et al. Diagnostic methods for Helicobacter pylori infection: Ideals, options, and limitations. Eur J Clin Microbiol. 2019; 38:55-66.
[Crossref] [Google Scholar] [PubMed]
- Rovaris GZ, Back JV, Ronchi-Colombo MP, Rosa VS, Cardoso MC, et al. Assessment of the accuracy of the rapid test for the diagnosis of Helicobacter pylori in patients that didn’t undergo previous eradication therapy and who went through endoscopy. Arq Gastroenterol. 2024; 61:e23136.
[Crossref] [Google Scholar] [PubMed]
- Qiu E, Li Z, Han S. Methods for detection of Helicobacter pylori from stool sample: Current options and developments. Braz J Microbiol. 2021; 52:2057-2062.
[Crossref] [Google Scholar] [PubMed]
- Yu M, Zhang R, Ni P, Chen S, Duan G. Helicobacter pylori infection and psoriasis: A systematic review and meta-analysis. Medicina. 2019; 55:645.
[Crossref] [Google Scholar] [PubMed]
- Choi IJ, Kim CG, Lee JY, Kim YI, Kook MC, et al. Family history of gastric cancer and Helicobacter pylori treatment. N Engl J Med. 2020; 382:427-436.
[Crossref] [Google Scholar] [PubMed]
- Koletzko L, Macke L, Schulz C, Malfertheiner P. Helicobacter pylori eradication in dyspepsia: New evidence for symptomatic benefit. Best Pract Res Clin Gastroenterol. 2019; 40:101637.
[Crossref] [Google Scholar] [PubMed]
- Bordin DS, Voynovan IN, Andreev DN, Maev IV. Current Helicobacter pylori diagnostics. Diagnostics. 2021;11:1458.
[Crossref] [Google Scholar] [PubMed]
- Wang YK, Kuo FC, Liu CJ, Wu MC, Shih HY, et al. Diagnosis of Helicobacter pylori infection: Current options and developments. World J Gastrointest. 2015; 21:11221.
[Crossref] [Google Scholar] [PubMed]