Case Report - Onkologia i Radioterapia ( 2025) Volume 19, Issue 12
Malignant Degeneration of a Pilonidal Sinus (Report of Two Cases)
Nejjari Sara*, Keita Diango, Alem Mehdi, El Hakym Samia, Oufrid Abir, El Hilali Hafssa, Chbihi Chaymae, Aabboub Basma, Amaadour Lamiae, Oualla Karima, Benbrahim Zineb, Arifi Samia and Mellas NawfelMorocco
Morocco
Morocco
Morocco
Morocco
Morocco
Morocco
Morocco
Morocco
Morocco
Morocco
Morocco
Nejjari Sara, Department of Medical Oncology, Oncology Hospital, Hassan II University Hospital, Faculty of Medicine, Pharmacy and Dentistry, Fez, Morocco, Email: sara.nejjari@usmba.ac.ma
Received: 01-Dec-2025, Manuscript No. OAR-25-175086; , Pre QC No. OAR-25-175086 (PQ); Editor assigned: 03-Dec-2025, Pre QC No. OAR-25-175086 (PQ); Reviewed: 19-Dec-2025, QC No. OAR-25-175086; Revised: 24-Dec-2025, Manuscript No. OAR-25-175086 (R); Published: 31-Dec-2025
Abstract
Pilonidal sinus disease is a common pathology in surgical practice. Chronic and neglected cases can result in malignant degeneration, a rare complication observed in approximately 1% of patients. Squamous cell carcinoma is the most common histological type, followed by basal cell carcinoma and mixed-type carcinoma. The first case was reported by Heinrich Wolff in 1900, describing a 21-year-old woman with two recurrences after surgical treatment of a pilonidal sinus. Although there were no initial signs of malignancy, the excised specimen after the second recurrence revealed squamous cell carcinoma. Since then, sporadic cases of pilonidal sinus carcinomas have been published globally in case reports and small series, with a total of approximately 140 cases reported in the literature to date. Various authors have reported a 5-year survival rate of approximately 55% to 61%, which is significantly worse than primary cutaneous squamous cell carcinoma. In this study, we report two cases of squamous cell carcinoma of the pilonidal sinus managed at the medical oncology department of CHU Hassan II in Fès, Morocco.
Keywords
Pilonidal sinus carcinoma; Squamous cell carcinoma; malignant degeneration; chronic pilonidal disease; Survival rate
INTRODUCTION
The malignant transformation of a pilonidal sinus is a rare but feared complication, and its prognosis is poor. The best treatment is undoubtedly early surgical excision of the primary lesion the progression of squamous cell carcinoma (SCC) arising from a pilonidal sinus from a localized surgical stage to an advanced non-surgical is approximately 0.1% to 1% of pilonidal sinus cases. We report two cases of squamous cell carcinoma complicating the evolution of pilonidal disease admitted and managed at the medical oncology department of CHU Hassan II in Fès, Morocco.
CASE REPORTS
Patient 1:
This is a 45-year-old male with a history of recurrent pilonidal sinus. His first pilonidal sinus abscess occurred in 2020, for which he underwent surgery. However, he experienced several recurrences, with the latest surgery in 2021 revealing well-differentiated keratinizing and infiltrating squamous cell carcinoma upon pathological examination [Figure 1]. Imaging showed no metastasis, but the patient was lost to follow-up for two years.
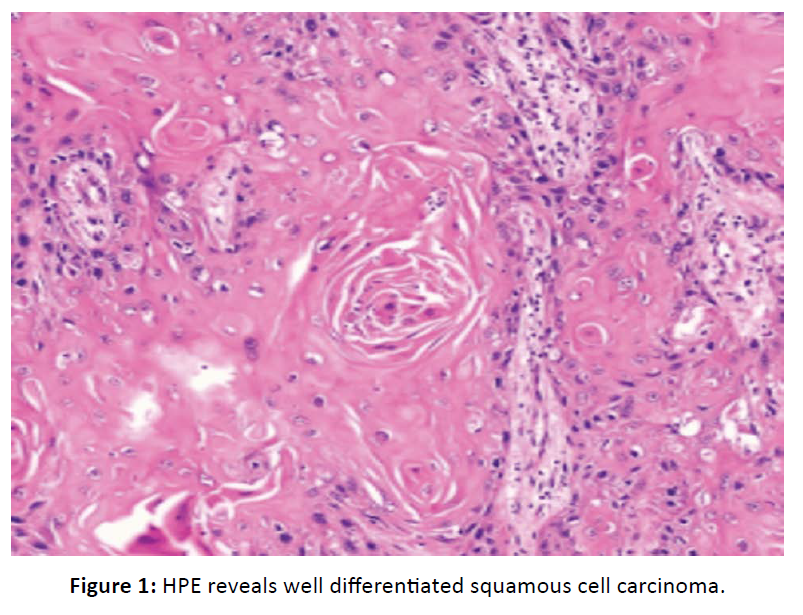
Figure 1: HPE reveals well differentiated squamous cell carcinoma.
On presentation to our department, clinical examination showed a large ulcerative lesion extending across the midline of the intergluteal region, with thickened and indurated edges and central necrosis. The surrounding skin demonstrated changes consistent with chronic inflammation. No palpable inguinal or femoral lymphadenopathy was identified [Figure 2].
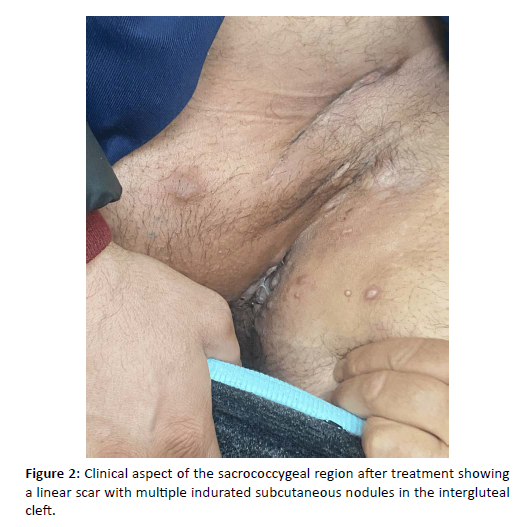
Figure 2: Clinical aspect of the sacrococcygeal region after treatment showing a linear scar with multiple indurated subcutaneous nodules in the intergluteal cleft.
A new imaging assessment revealed a mass involving the right gluteal region, compatible with locally advanced squamous cell carcinoma. Multidisciplinary discussion concluded that the lesion was unrespectable, and the patient was started on chemo radiotherapy over a 40-day period with concomitant capecitabine.
Six months after completing RCC, a CT scan revealed left inguinal lymph node involvement infiltrating the iliac muscle, as well as right external iliac and inguinal lymph nodes.
He was then placed on carboplatin AUC 5 in combination with paclitaxel. The patient received three treatment cycles, but the evaluation showed significant progression of secondary lymph node localizations. The patient died one week later before receiving a second-line treatment.
Patient 2:
This is a 32-year-old chronic smoker with a family history of neoplasms (mother with renal cancer, uncle with an undocumented hepatic tumor). On examination, the intergluteal fold showed several indurated nodules and healed scars consistent with repeated infections and sinus tracts. The area also displayed new firm nodular lesions with irregular surfaces, raising suspicion for malignant transformation in the context of chronic inflammation. No obvious ulceration was visible, but the firm, infiltrative texture of the nodules and progression despite conservative management prompted further evaluation [Figure 3].
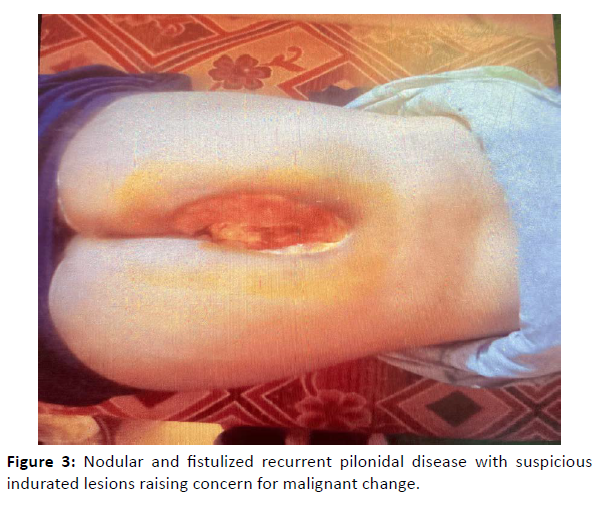
Figure 3: Nodular and fistulized recurrent pilonidal disease with suspicious indurated lesions raising concern for malignant change.
A biopsy-excision was performed, and the histopathological study favored moderately differentiated ulcerated squamous cell carcinoma with keratinization and infiltration. Pelvic MRI revealed a soft tissue tumor process in the sacro-gluteal region involving the sacral vertebrae S4 and S5, and the coccyx, measuring 32 x 45 mm in the axial plane, with a height of 70 mm. multiple satellite subcutaneous nodules were found along the intergluteal sulcus and retro coccygeal area, ranging in size from 13 to 20 mm. The tumor invaded the sacro-coccygeal ligament without bone involvement, along with a suspicious superior gluteal lymph node.
The patient underwent concurrent chemo radiotherapy, receiving a total dose of 66Gy/66Gy fractionated at 2Gy per session over two months. Follow-up pelvic MRI one month after RCC completion showed regression of the cutaneous and subcutaneous sacro-coccygeal infiltration, as well as the size reduction and necrosis of satellite nodules, but an increase in inguinal-pelvic lymph node size.
The patient was placed on systemic chemotherapy with cisplatin and 5-FU. He received only one cycle, with a clear clinical progression, and subsequently passed away.
DISCUSSION
Pilonidal sinus disease is a frequent condition of the sacrococcygeal region, typically affecting young, hirsute men and often associated with obesity, sedentary lifestyle, and deep natal cleft anatomy [1,2,3]. Although usually regarded as a benign inflammatory disorder, its chronicity, recurrent abscesses, and repeated surgical interventions may lead to significant morbidity and prolonged impairment of quality of life [1,2,3].
Malignant degeneration of a long-standing pilonidal sinus is an exceptional but severe complication. In the recent demographic overview by Safadi et al., approximately 140 well-documented cases of pilonidal sinus carcinoma were identified, with an estimated incidence around 0.1% among patients with pilonidal disease and a clear predominance of middle-aged men [4]. Earlier series and reviews, including those of Alarcón-del Agua et al. and Pilipshen et al., already emphasized that malignant transformation typically occurs after decades of chronic or recurrent disease, often in neglected or repeatedly relapsing sinuses [5,6]. More recent case reports and small series have confirmed this pattern and underlined the role of chronic inflammation and persistent infection as key carcinogenic drivers in this setting [7,8,9,10].
Histologically, squamous cell carcinoma (SCC) accounts for the vast majority of reported malignancies arising in pilonidal disease, whereas basal cell carcinoma, adenocarcinoma, and verrucous carcinoma remain exceptional [5,7,8,9,10]. Michalopoulou et al., Safadi et al., and Pyon et al. all described large ulcerative or vegetative lesions arising on a background of long-standing pilonidal disease, invariably showing well- to moderately-differentiated SCC on pathology [8,9,10]. In the survival analysis by Safadi et al., SCC histology, positive margins, and nodal disease were associated with worse outcome, highlighting the aggressive behavior of these tumors compared with primary cutaneous SCC of similar size [11].
Clinically, malignant transformation should be suspected in any chronic pilonidal sinus that becomes rapidly enlarging, indurated, ulcerated, or exophytic, especially when associated with bleeding, foul- smelling discharge, or unexplained pain. Sharma et al. and others have insisted that such changes in a long- standing sinus must prompt immediate biopsy [12,13,14]. Williamson et al. demonstrated that fine-needle aspiration cytology is a useful tool to document metastatic inguinal lymph-node involvement in this context, thereby facilitating staging and therapeutic planning [15]. As in our patient, cross-sectional imaging is essential to assess deep extension to sacrum, presacral fascia, rectum, or pelvic structures and to evaluate regional lymph nodes.
There is general agreement that wide en bloc excision with histologically negative margins represents the cornerstone of curative treatment whenever feasible [6,11,12-15]. De Bree et al. recommended excision including at least the presacral fascia, and, when necessary, partial sacrectomy or abdominoperineal resection for rectal involvement [15]. Large defects may require complex reconstruction using local or regional flaps as illustrated by Mayol Oltra et al. and others, who reported acceptable functional and oncological outcomes with multimodal strategies combining radical surgery and adjuvant radiotherapy [13,15]. Inguinal lymph-node dissection is indicated in the presence of clinically or radiologically proven nodal metastases, whereas prophylactic lymphadenectomy remains controversial and is not routinely recommended [11,15].
For patients with unrespectable loco regional disease or distant metastases, the therapeutic approach generally follows that of advanced cutaneous SCC. EGFR inhibition with cetuximab has shown meaningful response rates in phase II trials and small series, both as monotherapy and in combination with platinum- based chemotherapy, and may be considered for patients who are not candidates for immunotherapy or in whom immunotherapy has failed [16,17]. Jarkowski et al. summarized the experience with systemic agents in advanced cutaneous SCC, underlining modest but clinically relevant activity of cytotoxic chemotherapy and targeted therapy in this setting [18]. More recently, PD-1 blockade with cemiplimab has become a major advance: in a pivotal trial, Gross et al. reported high response rates, durable remissions, and favorable tolerability in patients with stage II-IV cutaneous SCC, leading to its adoption as a standard of care in international guidelines [19, 20].
Our case fits well within this spectrum of malignant degeneration: the patient had a long history of neglected pilonidal disease, presented with an extensive ulcerative mass and nodal involvement, and required multidisciplinary management. In line with available literature, the prognosis was driven less by the primary tumor than by regional spread and the difficulty of achieving clear margins in a functionally critical area [4,5,6,11,12-15,19,20]. This underscores two key messages for clinical practice: first, chronic or recurrent pilonidal disease, particularly in older patients, should never be considered purely benign; and second, any change in the clinical behavior of a pilonidal sinus (non-healing, recurrence after surgery, rapid growth, or atypical ulceration) must be regarded as malignant until proven otherwise, prompting early biopsy, complete staging, and referral to a specialized multidisciplinary team [4,5,10,11,19,20].
CONCLUSION
The degeneration of pilonidal disease into squamous cell carcinoma is a rare but feared complication. Close monitoring of patients with chronic inflammatory conditions in the pilonidal region is imperative to detect any malignant transformation early. The best treatment is undoubtedly early surgical excision of any pilonidal sinus.
References
- Esposito F, Lauro Mario, Tirone LP. Squamous cell carcinoma and pilonidal cyst disease. Ann. Ital. Chir. 2015; 86: S2239253X15023427. [Google Scholar], [PubMed]
- Mayol Oltra A, Boldó Roda E, Lozoya Albacar R, Morillo Macias V, Nobleja Quiles N. Squamous cell carcinoma over pilonidal chronic disease. A new therapeutic approach. Int. J. Surg. Case Rep. 2020; 70: 172-177. [Crossref], [Google Scholar], [PubMed]
- Safadi MF, Dettmer M, Berger M, Degiannis K, Wilhelm D, et al. Demographic overview of pilonidal sinus carcinoma: updated insights into the incidence. Int. J. Colorectal Dis. 2023; 38: 56. [Crossref], [Google Scholar], [PubMed]
- Safadi MF, Ghareb K, Daher A, Dettmer M, Shamma H, et al. Eight Patients With Pilonidal Carcinoma in One Decade-Is the Incidence Rising. Cureus. 2022; 14: e27054. [Crossref], [Google Scholar], [PubMed]
- Styliani N Parpoudi, Dimitrios S Kyziridis, Dimitrios Ch Patridas. Is histological examination necessary when excising a pilonidal cyst. Am. J. Case Rep. 2015; 16: 164‑ [Crossref], [Google Scholar], [PubMed]
- De Bree E, Zoetmulder FA, Christodoulakis M, Aleman BM, Tsiftsis DD, et al. Treatment of malignancy arising in pilonidal disease. Ann. Surg. Oncol. 2001; 8: 60‑ [Crossref], [Google Scholar], [PubMed]
- Matsushita S, Ohtake N, Mochitomi Y, Fukumitsu K, Nishi M, et al. A case of squamous cell carcinoma arising in a pilonidal sinus. J. Dermatol. 2002; 29: 757‑ [Crossref], [Google Scholar], [PubMed]
- Okuş A, Sevinç B, Karahan O, Eryilmaz MA. Comparison of Limberg flap and tension-free primary closure during pilonidal sinus surgery. World J. Surg. 2012; 36: 431‑ [Crossref], [Google Scholar], [PubMed]
- Kaya B, Eris C, Atalay S, Chauve Souris Ô. Modified Limberg transposition flap in the treatment of pilonidal sinus disease. Tech. Coloproctology. 2012; 16: 55‑ [Crossref], [Google Scholar], [PubMed]
- Humphries AE, Duncan E. Evaluation and management of pilonidal disease. Surg. Clin. North Am. 2009; 90: 1131242010. [Crossref], [Google Scholar], [PubMed]
- Konrad Wroński KX. A rare case of squamous cell carcinoma arising from chronic sacrococcygeal pilonidal disease. Ann. Ital. Chir. 2019; 8: S2239253X19030202. [Google Scholar], [PubMed]
- Dettmer M, Schumacher F, Matevossian E, Wilhelm D, Luedi MM, et al. Gender differences in axial hair strength may explain gender related incidence variation in Pilonidal Sinus patients. Pilonidal Sinus J. 7. [Crossref], [Google Scholar]
- Luedi MM, Schober P, Stauffer VK, Diekmann M, Andereggen L, et al. Gender-specific prevalence of pilonidal sinus disease over time: A systematic review and meta-analysis. ANZ J. Surg. 2021; 91: 1582‑ [Crossref], [Google Scholar], [PubMed]
- Kulaylat MN, Gong M, Doerr RJ. Multimodality treatment of squamous cell carcinoma complicating pilonidal disease. Am. Surg. 2020; 62: 922‑ [Google Scholar], [PubMed]
- Abboud B, Ingea H. Recurrent squamous-cell carcinoma arising in sacrococcygeal pilonidal sinus tract: report of a case and review of the literature. Dis. Colon Rectum. 1999; 42: 525‑ [Crossref], [Google Scholar], [PubMed]
- Velitchklov N, Vezdarova M, Losanoff J, Kjossev K, Katrov E. A fatal case of carcinoma arising from a pilonidal sinus tract. Ulster Med. J. 2001; 70: 61‑ [Google Scholar], [PubMed]
- Pekmezci S. Malignant degeneration: an unusual complication of pilonidal sinus disease. Eur. J. Surg. Acta Chir. 2001; 167: 475‑ [Crossref], [Google Scholar]
- Chatzis I, Noussios G, Katsourakis A, Chatzitheoklitos E, et al. Squamous cell carcinoma related to long standing pilonidal-disease. Eur. J. Dermatol. EJD. 2009; 19: 408‑ [Crossref], [Google Scholar], [PubMed]
- Sharma D, Pratap A, Ghosh A, Shukla VK. Malignant transformation of a pilonidal sinus. 2008; 145: 243‑ [Crossref], [Google Scholar], [PubMed]
- Gur E, Neligan PC, Shafir R, Reznick R, Cohen M, et al. Squamous cell carcinoma in perineal inflammatory disease. Ann. Plast. Surg. 1997; 38: 653‑ [Crossref], [Google Scholar], [PubMed]



