Case Report - Onkologia i Radioterapia ( 2023) Volume 17, Issue 1
Isolated cutaneous metastasis of scalp in breast cancer: A case-report
Fava Maria Giovanna1*, Francesca Maria Plutino2, Lorena Turano3, Francesco Messina3 and Del Medico Pietro42Unit of Pathological Anatomy-Great Metropolitan Hospital (G.O.M.), “Bianchi-Melacrino-Morelli Reggio Calabria, Italy
3Unit of Radiology-Great Metropolitan Hospital (G.O.M.) “Bianchi-Melacrino-Morelli” Reggio Calabria, Italy
4Unit of Oncology-Great Metropolitan Hospital (G.O.M.) “Bianchi-Melacrino-Morelli” Reggio Calabria, Italy
Fava Maria Giovanna, Unit of General Surgery-Great Metropolitan Hospital (G.O.M.) “Bianchi-Melacrino-Morelli”, Reggio Calabria, Italy, Email: mariagiovannafava@alice.it
Received: 26-Dec-2022, Manuscript No. OAR-22-84457; Accepted: 15-Jan-2023, Pre QC No. OAR-22-84457 (PQ); Editor assigned: 28-Dec-2022, Pre QC No. OAR-22-84457 (PQ); Reviewed: 10-Jan-2023, QC No. OAR-22-84457 (Q); Revised: 12-Jan-2023, Manuscript No. OAR-22-84457 (R); Published: 18-Jan-2023
Abstract
Breast Cancer (BC) is the most common malignancy to metastasize to skin in women with recent or late medical history of breast cancer.
Skin metastasis is a generic definition that includes a large grouping of different clinical situations.
In practice, it can be useful a clinical classification that divides cutaneous metastasis in short-term metastasis after a local treatment as local recurrences after conservative surgery and early stage-skin complications, such as nodular satellitosis associated with breastplate cancer or in located advanced and inflammatory breast cancer, distinctly in secondary skin metastasis associated to an Occult Breast Cancer (OBC) and in late cutaneous complications, if they occur after long-term period from a previous breast cancer history without breast-mass or nodule or without others secondary locations. The most important characterization is to distinguish breast cancer cutaneous locations in early or late metastasis.
Occult breast cancer that can be nearly to the breast region or in distant organs is characterized by metastatic presentation of undetectable breast tumour on imaging exams but it is a rare disease (accounting for 0.3% to 1.0% of all breast cancers) and represents a major diagnostic challenge. OBC has a better prognosis than a cutaneous metastasis case. In fact, it may exhibit spontaneous regression or respond to less aggressive treatment strategies as adjuvant therapy.
Inflammatory Breast Cancer (IBC) is a distinct and rare type of cutaneous breast cancer accounting for up to 6% of all breast cancer cases and, despite more aggressive treatments today, it is still a very serious disease with a high mortality.
In case of short-term metastasis or early-stage skin complications, correct diagnosis may be facilitated by anamnestic connection with the recent breast cancer.
Skin metastases are rare and are associated with a significantly higher rate of distant metastasis and uncontrolled local disease as well as a lower rate of survival.
Keywords
breast cancer, skin metastasis, tb-PET’s comparative applications, oncological approach, multidisciplinary consulting
Introduction
Skin metastasis may occur synchronously or metachronously with the diagnosis of a primary cancer, but occasionally they may represent an initial manifestation of an occult internal carcinoma. Breast cancer is one of the most common primary types of cancer that metastasize to the skin. In women metastatic cutaneous lesions exceed 20% of all cutaneous ones. The most common sites affected are the areas near the site of breast cancer, as chest wall’s skin or around surgical scar, but less commonly, skin metastasis can occur on other areas.
Skin metastases are different to local recurrence, which is when the primary breast cancer has come back in the breast area or near. The assessment of cutaneous metastatic disease can be perplexing, because the clinical presentation appears similar to other skin malignancies and require differentiation with benign dermatological disease.
If cutaneous metastasis occur after a long follow-up period from first breast disease, they can be considered very interesting under multiple aspects. Cutaneous breast carcinoma may arise as cutaneous metastasis or secondary to direct tumour extension to the skin (local recurrence).
Isolated distant cutaneous metastasis of breast carcinoma is more uncommon. Furthermore, an isolated single metastasis of the scalp seems to be very rare in breast cancer, as in our case. Although breast cancer has the highest cutaneous metastasis rate among internal malignancies, cutaneous metastasis actually occur in only a small minority of breast cancer patients.
The incidence of breast carcinoma cutaneous manifestation in patients with breast carcinoma is around 23%-24%.
The most common sites of breast carcinoma cutaneous manifestation are the chest wall and abdomen, but they can occur at the extremities and in the head/neck region.
In clinical practice, cutaneous metastases show a wide range of clinical manifestations and the presentation can be varied. Nodules are the most common presentation, but several other patterns are described as ulcerated lesion.
Scalp metastasis as the first sign of occult breast cancer or as initial presentation of a metastatic disease is an extremely rare condition and it is considered an atypical soft tissue metastasis [1]. Cutaneous metastasis from breast cancer typically carries a less unfavourable prognosis than cutaneous metastasis from other internal malignancies.
The recognition of cutaneous metastasis at an early stage is very important for the therapeutic approach.
A Case Report
We present a case of a woman (G.M.F. borned in 1948th) with an history of infiltrating ductal cancer of the left breast, status postmodified radical mastectomy 15 years prior.
The clinical and oncological history of the patient is very complex. T he woman was operated in a peripheral hospital in June 2007; she underwent to a breast biopsy of the left side with the histological report of infiltrating ductal carcinoma grading G2 moderately differentiated, associated with an intraductal carcinoma’s component comedo-type high grade. The immunohistochemical examination showed an Hormonal Receptor Status positive with ER percentage 75%, PgR 50%, a low proliferation’s index with Ki67 index 5% and Her-2 score 0. In that hospital, she underwent a quadrantectomy and an unspecified lymphoadenectomy, but after completing oncological surgery, the definitive histological report was negative for cancer. The patient started adjuvant hormonetherapy with anastrazole and she went for a radiotherapy’s visit in an another oncological centre, but here the specialists suspected a relapse’s persistence because of a mass-presence at the same breast left side.
In October 2007, the breast surgeon made a new wide-biopsy and the histological exam showed a high and medium grade intraductal carcinoma as papillary type, lobules’ cancerization, infiltrating ductal carcinoma’s diffuse microfoci, multiple papillomas and atypical hyperplasia. A radical left modified ma stectomy wa s performed; the final histological exam of the left breast was negative for cancer and “not ink on tumor” and clear margins for DCIS without residual disease, but the HER-2 level’s determination was score 2+ with amplification-FISH test negative. The women started chemotherapy from January 2008 to March 2008 with AC scheme (Adriamycin plus Cyclophosphamide) for 4 cycle-times. Radiological exams for oncological stadiation were negative and after 4 months, she started exemestane hormonal -therapy until march 2013. Finally she underwent to Radiotherapy treatment. T he woman followed up an close monitoring oncological program until 2013 without complications.
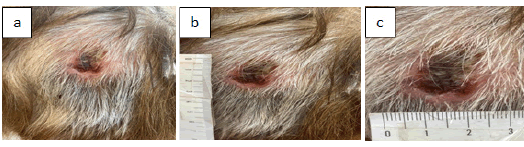
In May of 2022, the 75-year female patient with her personal history of malignant left breast carcinoma treated before (from 2007 to 2013) noticed a single cutaneous erythematous lesion in the scalp region and also a painful swelling in the second phalanx index finger of the left hand (Figure 1). The woman was referred to a Dermatology’ specialist for several months for the painless, immobile, hardened, skin-coloured mass fixed to the underlying tissues of the scalp. The scalp’s lesion measured 3 cm to 4 cm and was localized in the occipital region without evidence of regional lymphadenopathy in the neck. Because of highlighting the non –response pharmacological therapy and the lesion’s persistence, the woman contacted her breast surgery (Figure 1).
Figure 1: Metastatic cutaneous lesion of the scalp
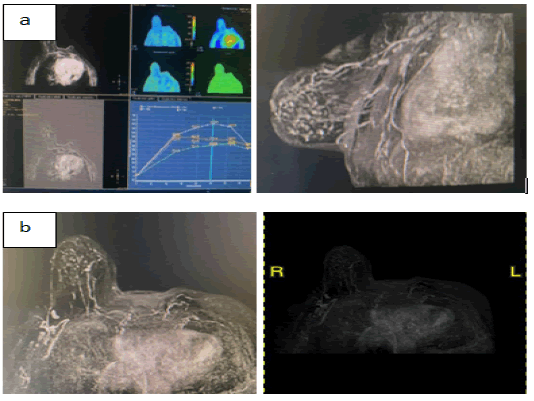
The biopsy test with immunohistochemistry results were positive for Hormone-Receptor status with estrogen receptor ER 90% and progesterone receptor PgR 90% but human epidermal growth factor receptor HER2 was negative. Pathology test showed a poorly differentiated carcinoma that was consistent with breast primary cancer. The Ki-67 proliferation index was high, around 20%, with an aggressive histological attitude, confirmed by endovascular carcinosis and perineural invasion in the microscopic sections. Imaging exams (mammography and ultrasonography of the right breast) did not show alterations-mass in the right side. The nuclear magnetic resonance (MRI) of the breast with contrast showed multiple lymphoadenopaties in the external superior quadrant at right side that radiologist send for further ultrasound informations (Figures 2) .
Figure 2: a.MRI with contrast of the Breast: b. Right breast and axillary region
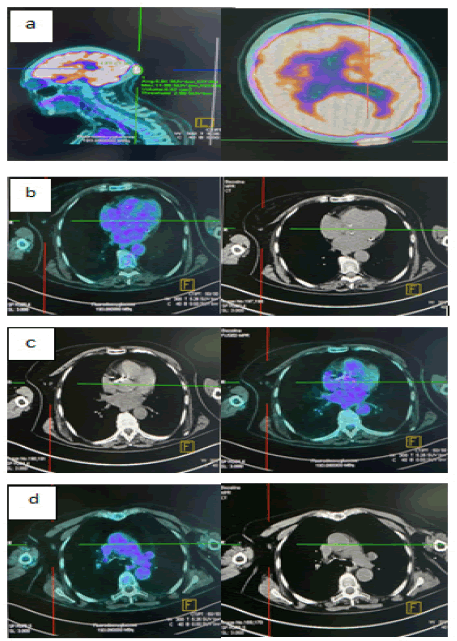
The total-body Positron Emission Tomography (tb-PET) showed an interesting finding, because the pathological uptake was in the skull case for the infiltrative lesion of the scalp, but a low metabolic activity was found in the right breast side indicating an enhancing micronodule at superior-external quadrant but a not significant activity in the axilla’s right lymphnodes. The nuclear medicine specialist underlined in his report that tb-PET exam has usually a low sensitivity for small size breast lesions’ detection and for also metastatic lymphnodes. A recommended radiological monitoring was chosen and the supervision senologist follow-up during next period was performed by targeted ultrasound checks (Figures 3).
Figure 3: Tb-PET exam: a. pathological uptake of the scalp; b. nodule in right breast side; c. lymphnodes in external superior quadrant in right side; d. lymphonodes in right axilla
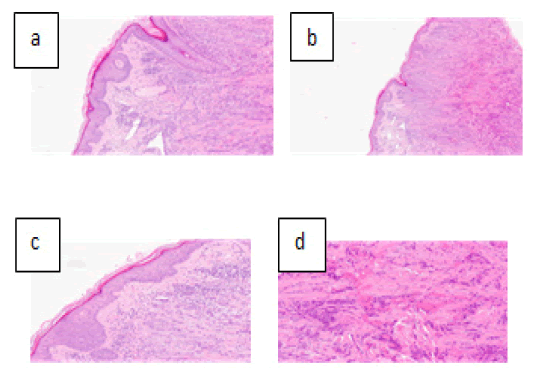
The woman had also an osteoarthritis with a painful swelling in her left hand’s finger. Histopathological examination and immune-histochemistry of the cutaneous scalp lesion confirmed the diagnosis of a metastatic breast carcinoma. The scalp lesion was compatible more likely with a long-distance recurrence, a late skin complication in the woman treated before in 2007 for the breast cancer hormone responsive bioprofile, which debunked an infiltrative bioprofile during the disease recurrence (Figures 4).
Figure 4: a. Histopatologic report: A Image-Microscope 10x; b. ImageMicroscope 4x; c. Endovascular carcinosis d. Perineural invasion.
Because of the small size of the right breast’s lesion showed by MRI and PET exams and the aspecific multiple activity of the right axillary lymphoadenopaty, no biopsy was performed, in according to the patient’s preferences, after a second oncological opinion, but the patient was placed in close follow-up without evidence of local changes in the right breast or others local recurrences.
After FM Giovanna , et al.- Isolated cutaneous metastasis of scalp in breast cancer: A case-report multidisciplinary consultation, the breast oncological specialists decided to start chemotherapy using fulvestrant 500 mg 1 in every 28 days and then ribociclid 600 mg for 3 weeks every month, but the hormonal treatment was stopped. At the last clinical examination, a clear regression in size and appearance of the single cutaneous lesion was evident, as viewed at the clinic (Figure 5). This positive evolution was confirmed by clinical follow-up and by the second t-b PET and the bone inflammatory phenomenon at left hand was stabilized by conservative method. No other breast lesion was detected with first and second-level radiological examinations and, in according with the oncologist, the patient is still continuing adjuvant chemotherapy, undergoing various clinical check-up and breast radiological monitoring up to the maximum therapeutic response; in future the scalp lesion will be surgically remove with a wide excision if not infiltrated the underlying tissue layers of the skull, for citoriductive purpose.
Figure 5: Post-I line chemotherapy: the scalp lesion’s clinical aspect
Discussion
Cutaneous metastasis may be the initial sign of internal malignancy but more often represents a late manifestation of a widely disseminated disease [2]. Breast carcinoma is the most common malignancy to metastasize to the skin. Cutaneous metastasis from breast cancer have varied presentations but there is no well-established classification which includes them all.
In practice, it can be useful a clinical classification that divides cutaneous metastasis in short-term metastasis after a local treatment as local recurrences after conservative surgery and early stage-skin complications, such as nodular satellitosis associated with breastplate cancer or in located advanced and inflammatory breast cancer, distinctly in secondary skin metastasis associated to an Occult Breast Cancer (OBC) and in late cutaneous complications, if they occur after long-term period from a previous breast cancer history without breast-mass or nodule or without others secondary locations. The most important characterization is to distinguish breast cancer cutaneous locations in early or late metastasis.
Metastasis is the multiple process by which an original primary tumor develops into a distal secondary tumour, and it is a representative hallmark of cancer and leads to treatment failure. In rare cases, skin metastasis may appear as the first clinical manifestation of breast cancer.
T he incidence of breast carcinoma cutaneous manifestation in patients with breast carcinoma is around 23%-24% [3]. Scalp metastasis as the first sign of occult breast cancer or as initial presentation of a metastatic disease is an extremely rare condition, as in our case-report, and it is considered an atypical soft tissue metastasis.
Distant cutaneous metastasis show a predilection for the contralateral anterior chest wall area, followed by the head and neck, back and abdomen. Histologically, most of the tumours presented in this series (both ipsilateral and distant metastasis) demonstrate features of infiltrating ductal carcinoma with little change in histologic features from the primary lesion; however, the distant metastasis show a tendency to display more poorly differentiated features, as in our case report.
Metastasis is a multistep complex process that requires the cooperation of tumour cells, tumour microenvironment and target tissues of metastasis, involves multiple cellular mechanisms. Metastatic breast cancer cells often acquire aggressive characteristics through several mechanisms, and develop an high proliferation index compared to the previous hormonal subtype at the first diagnosis. It is known the relevant genetic polymorphisms underlying complex phenotypes in breast cancer and germline genetic variants influence metastasis development, but it‘s also clear that host’s genetic makeup facilitates metastases by the dysregulation of gene expression that can promote the metastatic dispersion.
The clinical spectrum of the skin metastatic disease can mimic benign conditions. The diagnosis depends on thorough clinical examination and complementary exams as biopsy that is mandatory. Patients often turn to the dermatologist, that don’t know how to make differential diagnosis, causing a delay in starting adequate therapies.
There is no “standard of care” on management of skin metastatis. In particular, the role of surgery in the treatment of cutaneous metastasis from breast carcinoma remains controversial [4, 5].
A wider comparison of the clinic-pathologic features of patients with skin’s metastasis is necessary and it might be develop on a major group to suggest an alternate biological mechanisms applied for local and distant skin metastases from breast carcinoma and the more suitable multidisciplinary approach in personalized therapy.
In rare cases, cutaneous metastasis appears as the first clinical manifestation of breast cancer. It is therefore crucial for patients and health professionals alike to be aware of new skin lesions. Cutaneous metastasis is a diagnostic sign of cancer that is not restricted exclusively to later forms of the disease. Usually, when the skin is affected by metastases, other organs have already been involved marking the former as a sign of poor prognosis and women with a simultaneous diagnosis of cutaneous and visceral metastases have the shortest survival and poor prognosis because of aggressive systemic disease. A single skin lesion is a treatable condition if a right diagnostic-therapeutic pathway is traced.
Scalp metastasis from breast cancer is an exceedingly infrequent phenomenon [6]. Skin involvement can be in the form of nodules and purpuric papulo-vesicles on a background of erythema which clinically mimicked lymphatic malformation. The nodules vary in size and appear as hardened lesions, either single or multiple, located on dermis and subcutaneous tissue, as observed on the patient in question, but their color can be also similar to that of normal adjacent skin and they can be asymptomatic. On occasion, lesions may erode and ulcerate secondary to the tumoral mass pressure on cutaneous surface. The most frequent histopathologic pattern in cutaneous metastasis is the enlarged nodule, located on the deeper dermis, adjacent to or inside its intersection with the subcutaneous tissue.
Therefore, although rare in dermatologists' clinical practice, cutaneous metastasis of breast cancer are clinically important, because their immediate detection may contribute to reduce associated morbidities and mortality. Prompt diagnosis is crucial, as it will have future implications, particularly regarding prognosis and treatment.
Skin metastasis can be suspected and recognized earlier through physical examination than metastasis in other internal organs or systems but they are a diagnostic challenge due to the variable clinical presentation. A high index of suspicion is mandatory for a prompt diagnosis. Skin biopsy of such lesions is an important step to confirm the diagnosis and, in the right clinical scenario, it can provide informations on the primary origin of the tumour. Because it indicates a systemic relapse, it is necessary to intervene with intravenous chemotherapy, to which local therapies can be associated. Surgery of a limitated skin lesion may be performed but it is not possible for an advanced stages or for an infiltrating lesion.
Usually, treatment for metastatic cancer to skin involves treating the underlying cancer, but the most appropriate therapy could include different approaches as surgery, chemotherapy and radiation-therapy that alternate at different times. The prognosis of this condition depends on the severity of signs and symptoms, the number of organs systems affected and the response to various treatments [7].
Conclusion
The study and the diagnostic framing of the metastasis’ status in breast cancer is an important process that can be both a therapeutic target and a detectable marker.
Individuals, who respond well to adjuvant therapies as in our casereport, have better prognosis than those who do not respond to systemic treatment, but the prognosis is usually poor because skin metastasis often indicates a high-stage cancer. When metastasis occurs to the skin from breast cancer, other organs may already have been affected; rarely as in this case, it may be the first and the only sign of cancer recurrence even after late –period.
In the case-report, no other breast lesion was detected after this chemotherapy’s scheme, and the patient is still continuing adjuvant therapy, undergoing various clinical check-up and breast radiological monitoring up to the maximum therapeutic response . At the moment, the scalp lesion doesn’t cause discomfort but only disfigurement to the patient. The scalp lesion will be surgically remove in future with a wide excision if not infiltrated the underlying tissue layers of the skull, for a citoriductive purpose, after completing the treatment, because removal of the skin lesion may enhance the patient’s quality of life and, if it remains the one and only single lesion without distant metastasis, surgical excision could have little positive effect on the final outcomes for patient.
It is very important to quickly identify the first metastasis, because the prognosis in these cases is very good, as our case shows.
Targeted therapeutics for breast cancer include substances or drugs that block cancer growth by interfering with the function of certain molecules responsible for tumor cell proliferation and survival. In particular, personalized treatment for individual patients can enhance the therapeutic efficacy and minimize chemotherapy-induced toxicity in breast cancer, but a multidisciplinary consultation is necessary for a correct diagnostic picture and the treatment success.
Conflict of Interest
The authors declare that there are no competing interest.
References
- N Alizadeh, H Mirpour, S Z Azimi: Scalp metastasis from occult primary breast carcinoma: A case report and review of the literature; Int J Womens Dermatol 2018 ;4:230-235.
- V A Ferreira, K Spelta, L Martins Diniz, E A Lucas: Exuberant case of cutaneous metastasis of breast cancer ; An Bras Dermatol 2018;93:429-431.
- Bittencourt M J S , Carvalho A H, Nascimento B A, Freitas L K M, and Parijós A M: Cutaneous metastasis of a breast cancer diagnosed 13 years before. An Bras Dermatol 2015; 90: 134–137.
- Huang S, Parekh V, Waisman J, Jones V, Yuan Y, et al: Cutaneous metastasectomy: Is there a role in breast cancer? A systematic review and overview of current treatment modalities. J Surg Oncol 2022 Aug ;126(2): 217–238.
- Liu YF, Liu LY, Xia SL, Li T, Li J: An unusual case of Scalp Metastasis from Breast Cancer . World Neurosurg 2020;137: 261-265.
- P R Cohen: Pleomorphic appearance of breast cancer cutaneous metastases. Cureus 2021;[ Google Scholar]
- Danforth DN, Aloj L, Carrasquillo JA, Bacharach SL, Chow Cet al: The role of 18F-FDG-PET in the local/regional in women with breast cancer. Breast Cancer Res Treat 2002; 75:135-146. ;[ Google Scholar]