Case Report - Onkologia i Radioterapia ( 2023) Volume 17, Issue 8
Hemi-nephrectomy for renal malignancy in patients with horseshoe kidney : A case report
Arber Neziri1,3, Luljeta Neziri-Ahmetaj2*, Avni Fetahu3, Ferdinand Komani3, Sabit Mehmeti3 and Musa Oruqi32Medical Faculty ”Hasan Prishtina” Prishtinë Department of Physiology and Immunology, Kosovo
3Urology Clinic, University Clinical Centre of Kosovo, Pristina, Kosovo
Luljeta Neziri-Ahmetaj, Medical Faculty ”Hasan Prishtina” Prishtinë Department of Physiology and Immunology, Kosovo, Email: luljetaneziriahmetaj@gmail.com, luljetaahmetaj@uni-pr.edu
Received: 26-May-2023, Manuscript No. OAR-23-100103; Accepted: 15-Sep-2023, Pre QC No. OAR-23-100103 (PQ); Editor assigned: 24-Jun-2023, Pre QC No. OAR-23-100103 (PQ); Reviewed: 18-Jul-2023, QC No. OAR-23-100103 (Q); Revised: 25-Aug-2023, Manuscript No. OAR-23-100103 (R); Published: 02-Sep-2023
Abstract
Introduction: Horse Shoe kidney (HSK) is the most common fusion anomaly, with an incidence rate of 1 in 400 of the general population. While most of the reported cases are incidental findings, sometimes a patient may present with pictures of hydronephrosis, infection, and calculus formation. In these patients, nephron-sparing surgical management of renal tumour s may be complicated by abnormal renal location, aberrant vasculature, and the presence of a renal isthmus.
Case Report: Forty six-old male patient was admitted to our outpatient clinic with a 10 cm suspicious mass in the horseshoe kidney that was detected during an attack of acute abdominal pain and haematuria. Computed tomography revealed a heterogeneous hypodense lesion containing renal tumour of 100 mm x 100 mm x 85 mm in size in upper pole at left kidney. Partial nephrectomy was performed non-ischemically Pathological examination revealed stage carcinoma urothelialis high grade with a negative surgical margin. During follow-up; urea, creatinine, and glomerular filtration rate were found to be normal.
Conclusion: The incidence of renal cell carcinoma in horseshoe kidneys is the same as in normal kidneys, and its development and course are not associated with the presence of the defect. According to the literature, transitional cell carcinoma is more common in horseshoe kidneys. This may be due to the presence of defects such as urinary obstruction, affiliation for nephrolithiasis, and chronic infection.
Keywords
horseshoe kidney, nephrectomy, transitional cell carcinoma
Introduction
Horseshoe kidney is the most common fusion anomaly, with an incidence rate of 1 in 400 of the general population [1]. While most of the reported cases are incidental findings, sometimes a patient may present with pictures of hydro nephrosis, infection, and calculus formation [2]. Rarely, a patient presents with malignancy of the renal unit.
Case Presentation
A 46-year-old male patient presented to our urologic department with a chief complaint of a multiple episode of painless, total gross haematuria, first time before 6 months. There was history of flank pain, dysuria, fever, but without weight loss or anorexia.
On physical examination, an ill-defined lump 10 cm × 10 cm was palpable in the upper left quadrant involving the left lumbar and umbilical regions. The baseline blood investigations were within the normal limit. His urine examination revealed 30-35 RBC/ HPF. An ultrasonography of the abdomen indicated the presence of HSK with a mass approximately 10 cm × 10 cm arising from the upper pole of left renal moiety.
The multi detecting Computer Tomography (CT) scan confirmed the presence of a horseshoe kidney with fusion at the lower pole, an enhanced lesion of 10 cm × 10 cm arising from the upper pole of the left renal moiety (Figure 1).
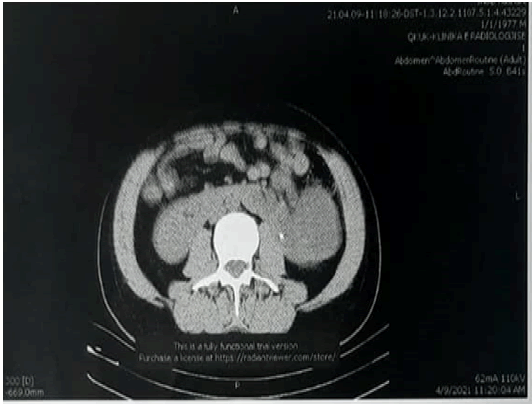
Figure 1: A CT scan showing the tumour from the upper pole of the left renal side of a horseshoe kidney
The metastatic work-up, which included a chest X-ray and liver function test, was normal. No significant lymphadenopathy was noticed (Figure 2).
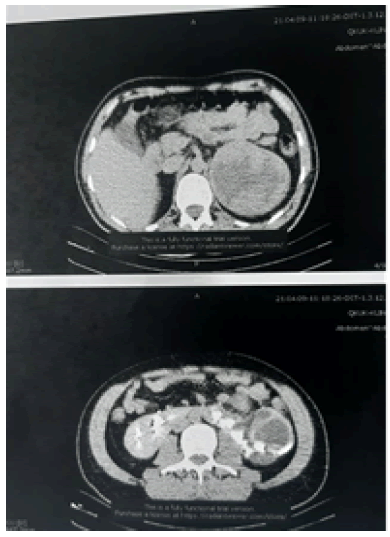
Figure 2: A CT scan showing the tumor from the upper pole of the left renal side of a horseshoe kidney
The patient underwent right radical nephrectomy with isthmectomy by the median trans-peritoneal approach. Intraoperatively, the finding of a horseshoe kidney with a mass arising from the right upper pole was confirmed (Figure 3).
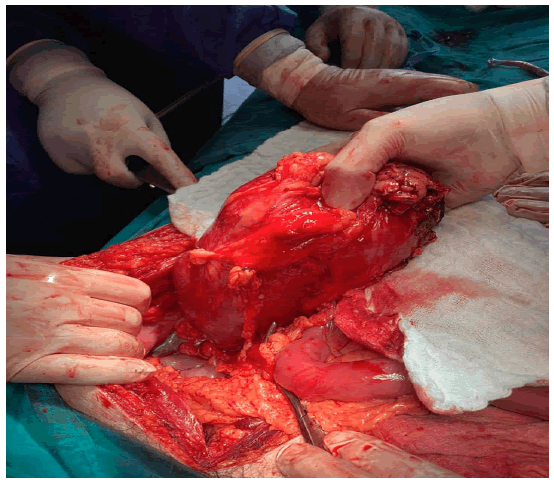
Figure 3: A CT scan showing the heminephrectomy for renal tumor of the left renal side of a horseshoe kidney
A well-formed isthmus was found connecting to the lower pole. The stump of the isthmus was run under with an absorbable running suture, and then it was covered with an omental patch to prevent haemorrhage and urinary fistula formation.
Postoperative recovery was very fast and the patient was discharged on the fifth postoperative day. The microscopic diagnosis was urothelial carcinoma high grade with no invasion of the capsule and negative surgical margins.
The patient is under regular postoperative surveillance without any local recurrence or metastatic activity after 20 month postoperative.
Discussion
Horseshoe kidney is the most common fusion anomaly, with an incidence of 0.25% in the general population. It is found to be more frequent in men, with a 2:1 male/female ratio [1, 2].
There are several variations in the basic shape of the horseshoe kidney. In 95% of cases, the kidneys join at the lower pole, which occurs before the kidneys have rotated on their long axes. In a small subset, an isthmus connects both upper poles [3-6].
Because of the increased use of ultrasound screening most of the time it is diagnosed incidentally. However, it is rare that a patient presents with malignancy of the renal unit.
About 150 patients with horseshoe kidney presenting with malignancy of the renal unit have been reported [7]. Of all the reported cases, renal cell carcinoma accounts for about half of the cases] while renal pelvic tumour s and Wilms tumour account for the remaining 50% (with equal incidence) [4, 8-10]. Rarely, sarcoma and carcinoids have been reported. The incidence of RCC in horseshoe kidney is no greater than that in the general population, but renal pelvic tumour and Wilms tumour are greater. Except for renal pelvic tumour s, most of the renal malignancy in HSK arises from the isthmus [9-11].
During the operation, the division of the isthmus is essential, not only to achieve complete access to the lymph nodes, but also to normalize the course of the ureter and to prevent the potential development of rovsing syndrome [11]. Survival from this tumour s is related to the pathology and the stage of the tumour at diagnosis, and not to the renal anomaly [12]. In our case series, survival seems to be good since the tumour was localized and didn’t involve perinephric fat or any adjacent structure.
Conclusion
Horseshoe kidney is the most common renal fusion anomaly and is more predominate in males and it is detected as incidental finding on CT or US examination. Urothelial carcinoma is one of the malignancies associated with horseshoe kidney, as was seen in our case.
References
- Bitkin A. Laparoscopic Nephrectomy in Patients with Congenital Kidney Anomalies: Single-Centre Results. J Reconstr Urol. 2018; 8.
- Glenn JF. Analysis of 51 patients with horseshoe kidney. N Engl J Med. 1959; 261:684-687.
- Hildebrand O. Beitrag zur Nierenchirurgie. Dtsch. Z. Chir. 1895; 40:90-149.
- Briones JR, Pareja RR, Martín FS, Toniolo GC, Pérez JH, et al. Incidence of tumoural pathology in horseshoe kidneys. Eur Urol. 1998; 33:175-179.
- Benjamin JA, Schullian DM. Observations on fused kidneys with horseshoe configuration: the contribution of Leonardo Botallo (1564). J Hist Med Allied Sci. 1950; 5:315-226.
- Love L, Wasserman D. Massive unilateral non-functioning hydronephrosis in horseshoe kidney. Clin Radiol.1975; 26:409-415.
- Meredith F. Campbell, Alan J. Wein, Louis R. Kavoussi. Campbell-Walsh Urology, 10th edition.
- Romics I., P Riesz. Bilateral renal cell carcinoma in a horseshoe kidney. Pathol Oncol Res. 2002; 8: 270-271.
[CrossRef]
- Miyazaki Y, Miyajima A, Maeda T, Ito Y, Tanaka N, et al. Renal cell carcinoma arising from a horseshoe kidney in a chronic hemodialysis patient. Clin Exp Nephrol. 2012; 16:647-651.
- Tanaka T, Koie T, Iwabuchi I, Ogasawara M, Kawaguchi T, et al. Primary leiomyosarcoma of a horseshoe kidney in a woman with Turner syndrome: a case report. BMC Res Notes. 2014; 7:1-4.
- Hohenfellner M, Schultz-Lampel D, Lampel A, Steinbach F, Cramer BM, et al. Tumour in the horseshoe kidney: clinical implications and review of embryogenesis. J Urol. 1992; 147: 1098-1102.
- Murphy DM, Zincke H. Transitional cell carcinoma in the horseshoe kidney: report of 3 cases and review of the literature. Br J Urol. 1982; 54:484-485.



