Research Article - Onkologia i Radioterapia ( 2022) Volume 16, Issue 2
Feasibility and therapeutic implication of computed tomography-guided TruCut biopsy in cases of recurrent adenocarcinoma lung
Sagar Varotaria1, Satya Sundar Gajendra Mohapatra1, Adya Kinkar Panda1, Soumya Surath Panda2 and Lalatendu Moharana2*2Department of Medical Oncology, IMS and SUM Hospital, Bhubaneswar, India
Lalatendu Moharana, Department of Medical Oncology, IMS and SUM Hospital, Bhubaneswar, India,
Received: 20-Jan-2022, Manuscript No. M-51941; , Pre QC No. P-51941; Editor assigned: 22-Jan-2022, Pre QC No. P-51941; Reviewed: 15-Feb-2022, QC No. 51941; Revised: 28-Feb-2022, Manuscript No. 51941; Published: 10-Mar-2022
Abstract
Introduction: Recurrence is a rule, in the case of advanced NSCLC and even patients with early-stage disease are at risk of disease recurrence. It is recommended to acquire tissue biopsy samples at recurrence, not only for the diagnosis of relapsed disease but also for additional molecular analysis. TruCut biopsy is a simple procedure, is relatively safe, rapid and a reliable technique for the diagnosis of lung lesions. But all patients may not be ideal candidates for needle biopsy at recurrence because of various tumour related and patientrelated factors. This study of ours tried to find out the feasibility of image-guided transthoracic needle biopsy and compared its therapeutic implications with those who could not undergo the procedure.
Result: Overall adequacy rate of obtaining tissue samples was 89.7% (35/39). All patients who undergo needle biopsy tolerated it well. Most common complications were pneumothorax (12.8%) (5/39) and pulmonary haemorrhage (10.2%) (4/39). Two (5.1%) patients developed hydropneumothorax. The cumulative percentage of side effects was 17.9% (7/39) and no procedurerelated fatality. 42.8% of patients who underwent needle biopsy were started with the second line targeted/Immunotherapy. Only 21.0% of the patients who underwent liquid biopsy instead, received targeted therapy in the second line.
Conclusion: TruCut biopsies of NSCLC’S at recurrence are feasible and are adequate in appropriately selected patients and associated with acceptable rates of complications. Rebiopsy may explore new tumour characteristics and give the opportunity to act on changes in tumour behaviour. For those patients who are not candidates for a needle biopsy, in them, liquid biopsy is a comparable alternative.
Keywords
recurrent lung cancer, repeat needle biopsy, liquid biopsy
Introduction
Lung cancer is one of the leading causes of cancer deaths worldwide. The common histologic types are Adenocarcinoma (ADC), Squamous Cell Carcinoma (SCC) and Small Cell Lung Cancer (SCLC). Clinical staging is performed with noninvasive diagnostic modalities, such as total body CT scan with contrast, and/or Positron Emission Tomography (PET). Diagnostic tissue biopsies may be obtained through percutaneous route with image-guided needle biopsy or bronchoscopic biopsy for endobronchial lesions or open biopsy if the former modalities could not obtain tissue. TruCut biopsy is a simple procedure, is relatively safe, rapid and a reliable technique for the diagnosis of lung lesions, particularly with the aid of a Computed Tomography (CT) scan [1]. Core biopsy not only distinguishes between benign and malignant lesions but also helps in tumour typing and molecular characterization of lung cancers, so customised targeted treatment is possible according to the tumour types. A common concept, in oncology as in microbiology, is that prolonged exposure to certain drugs can select a resistant population, either a neoplastic cell or a bacterium. Acquired resistance limits the great hopes of targeted therapies as well. The majority of patients experience it after a variable interval of time, because of a resistant clone that causes disease progression. A deeper understanding of molecular biology has made it possible in some cases to identify the specific mechanisms behind acquired resistance. So it is recommended to acquire tissue biopsy samples at recurrence, not only for the diagnosis of relapsed disease but also for additional molecular analysis [2,3]. Molecular analysis can be performed on surgical specimens, cytology cell blocks or small tissue biopsy specimens taken from the primary tumour or metastases. As needle size increases, the risk of complications also increases. Risk also depends on the location of the tumour. The most common complications include pneumothorax and bleeding. In case tissue is not obtainable, for molecular characterization of the recurrent disease, newer modalities like liquid biopsies such as Circulation Tumour Cells (CTC) or circulating tumour DNA (ctDNA) assays are promising alternatives [4,5]. So in this study, we tried to determine the feasibility and safety of CT guided lung biopsy of relapsed NSCLC and tried to determine its therapeutic implications, in comparison to where tissue biopsy was not feasible. Our aim here is to determine the feasibility and safety of CT guided lung biopsy of NSCLC (Adenocarcinoma) at recurrence. Finer molecular characterization through nextgeneration sequencing and immunohistochemistry and to find out the pros and cons of image-guided lung biopsy in comparison to liquid biopsy.
Methodology
Sixty-six non-small cell lung cancer (Adenocarcinoma) patients irrespective of the stage of presentation, who were being treated in our hospital, were enrolled in the study and followed up prospectively. Over time 12 patients were lost to follow up. All of the 54 patients on follow up eventually had recurrence/ progression of the disease, which was documented with contrast, enhanced CT scan. All of them were evaluated for trans-thoracic CT guided needle biopsy at progression. The feasibility of needle biopsy was studied according to the various tumour and patient-related factors and reasons for not being able to conduct needle biopsies were documented. Patients in whom, a needle biopsy was not possible for whatever reasons, were subjected to liquid biopsy. Between the liquid biopsies and needle biopsies, therapeutic implications were compared.
Pre-procedure evaluation and the procedure
Prothrombin Time (PT), International Normalized Ratio (INR), Activated Partial Thromboplastin Time (APTT), and platelet count was checked before a needle biopsy. Those patients, who were on aspirin or clopidogrel, were asked to discontinue it 5 days before the biopsy. Patients on oral anticoagulants were switched to low molecular weight heparin before 3 days, which in turn was withheld on the day of the procedure. CT studies were performed on 128 SLICE CT SCANNER [GE OPTIMA CT660] in all patients. Location of the lesions, location of fissures adjacent to the lung lesions or within the pathway of the biopsy needle trajectory, location of adjacent arteries and
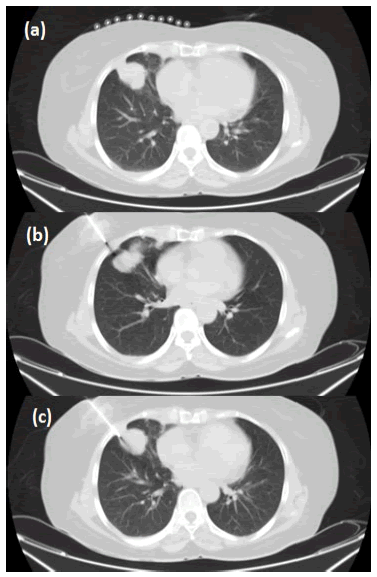
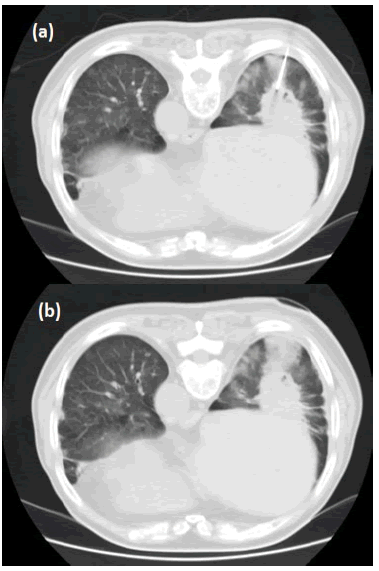
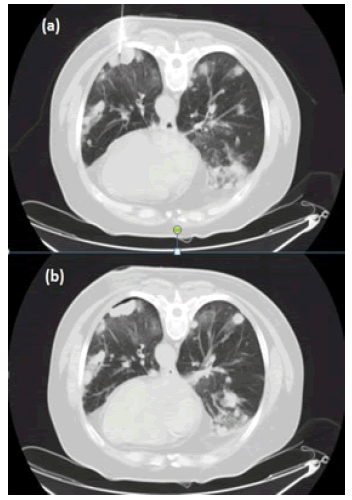
veins were evaluated, in order to plan the needle trajectory. The angle of entry of the needle, route of entry and distance between skin and the lesion and the length of throw was documented on the CT scan monitor. Patients were positioned either in prone, supine or lateral position depending on the skin site entry point chosen. The breath-holding technique was followed during the procedure and it was explained to the patient and was practised beforehand. Patients were asked to avoid coughing and taking deep breaths during the procedure (Figures 1-3).
Figure 1: Representative case of percutaneous transthoracic core needle biopsy in a Relapsed NSCLC patient. Axial CT image (lung window) (5 mm section thickness) shows a mass in the right middle lobe; (a): Surface Markers; (b): Coaxial needle approach; (c): Advancement to lesion-Repeat CT scan obtained after needle insertion ensures that the needle tip (arrow) is located within the target mass
Figure 2: Representative case of percutaneous transthoracic core-needle biopsy in a Relapsed NSCLC. Patient. Axial CT image (lung window) (5 mm section thickness) shows mass in the right lower lobe; (a): Repeat CT scan obtained after needle insertion ensures that the needle tip (arrow) is located within the target mass; (b): Post Procedure-Pulmonary Hemorrhage
Figure 3: Representative case of percutaneous transthoracic core needle biopsy in a Relapsed NSCLC patient. Axial CT image (lung window) (5 mm section thickness) shows a mass in the left lower lobe (a case of multicentric recurrence); (a): Repeat CT scan obtained after needle insertion ensures that the needle tip (arrow) is located within the target mass; (b): Post Procedure-Minimal Pneumothorax.
Statistical evaluation
Quantitative data is represented in form of a percentage. Data analysis was done using Statistical Package for Social Sciences (SPSS) version 25.0.
Results
Baseline patient and tumour characteristics are mentioned in Table 1. All of the 54 patients on follow up eventually had recurrence/progression of the disease. Forty-six (n=46) of these 54 patients had a recurrence in the lung with or without other sites of metastasis. And the rest 8 patients had recurrences at distant sites only and did not involve lung at recurrence. Out of the 46 patients who had lung lesions at recurrence, 39 patients underwent trans-thoracic needle biopsy. Among them, viable tumour tissue could be obtained for 35 patients. Among the 7 patients who did not undergo needle biopsy, 3 had a poor general condition with low oxygen saturation. For 4 patients, lung lesions were close to the great vessels, which made them unfit for needle biopsies. Patients in whom viable tissue could not be acquired through needle biopsy, or whose who could not undergo needle biopsy because of technical issues, or those who did not have a lung lesion at recurrence and other lesions were not amenable for biopsy, were subjected to liquid biopsy.
Tab. 1. Patient characteristics
|
Characteristics |
N=54 |
|
|
Sex |
|
|
|
|
Male |
32 |
|
|
Female |
22 |
|
Age (in years) |
|
|
|
|
Median |
63(29-87) |
|
Primary treatment |
|
|
|
|
CT+RT |
12 |
|
|
Palliative chemotherapy |
20 |
|
|
TKIs |
34 |
|
Sites of disease on recurrence/progression |
|
|
|
|
Lung ± others |
46 |
|
|
Other sites without lung lesion |
8 |
|
Location of the largest lung lesion |
|
|
|
|
RUL |
12(26%) |
|
|
RML |
6(12%) |
|
|
RLL |
10(22%) |
|
|
LUL |
11(24%) |
|
|
LLL |
7(16%) |
Discussion
The study was conducted with the objective to determine the feasibility and safety of CT guided TruCut biopsy in recurrent NSCLC (adenocarcinoma) patients. Out of 46 patients who had lung lesions at recurrence, rebiopsy was performed in 39(84.7%) patients, 7(15.3%) patients did not undergo biopsy due to the limiting factors such as poor performance status and difficult location of the tumour. Out of 39 patients who underwent needle biopsy, adequate tumour tissue could not be obtained in 4(10.3%) patients. So the adequacy rate of obtaining tissue samples was 89.7% (35/39). All patients who underwent needle biopsy tolerated well, cumulative percentage of side effects was 17.9% (7/39) and no procedure-related fatality (Tables 2 and 3) (Figures 2 and 3). According to studies, pneumothorax has been reported to be the most common complication of needle biopsy of the lung lesions and is reported to occur in 17%-27% of patients; pulmonary haemorrhage is the second most common complication, with reported frequencies ranging from 4%-27% [6-10]. Our complication rates for pneumothorax (12.82%) and pulmonary haemorrhage (10.25%) were comparable to the above-mentioned studies. Patients treated with EGFRTKIs, frequently leads to the appearance of drug-resistant mutations within the target kinase [11-13]. A few of these new mutations are targetable, so the molecular characterisation of the additionally acquired mutations is the need of the hour. In our study, there was no statistically significant difference in the probability of finding a driver mutation or a resistance causing mutation like T790M, between needle biopsy and liquid biopsy. But in comparison to the liquid biopsy, a needle biopsy can procure tissue for histopathologic examination and IHC, so can detect histologic transformations or second primary if any, as well (Table 2). 42.8% (15/35) of patients who underwent needle biopsy were started with the second line targeted/ Immunotherapy. Only 21.0% (4/19) of the patients who underwent liquid biopsy instead, received targeted therapy in the second line.
Tab. 2. Results of molecular analysis
|
|
Needle biopsy at recurrence (n=35) |
Liquid biopsy at recurrence (n=19) |
P* |
|
EGFR exon 19 mutation |
13 |
9 |
P value not significant |
|
EGFR exon 21 (L858R) |
6 |
6 |
|
|
EGFR Exon 20(T790M) |
5 |
9 |
|
|
PD L1 |
7 |
X |
|
|
ALK rearrangement |
2 |
X |
|
|
ROS1 |
1 |
X |
|
|
BRAF (V600E) |
2 |
X |
|
|
*Chi-square test |
|||
Tab. 3. Complications in rebiopsies performed in relapsed cases of Non-small cell lung cancer
|
Complications |
(n=39) |
Percentage |
|
Pneumothorax |
5 |
12.82% |
|
Pulmonary Hemorrhage |
4 |
10.25% |
|
Hydropneumothorax |
2 |
5.12% |
|
No complication |
32 |
82.05% |
Conclusion
Rebiopsy and mutational analysis of NSCLC’S are feasible and are adequate in appropriately selected patients and associated with acceptable rates of complications. Rebiopsy may explore new tumour characteristics and give the opportunity to act on changes in tumour behaviour. Rebiopsy can be used to predict therapeutic resistance and consequently redirect targeted therapies. Thus changes in treatment facilitate better tumour control. For those patients who are not candidates for a needle biopsy, in them, liquid biopsy is a comparable alternative.
References
- Sidoun Mohamed M, Topov Y, Elfageh MA, Mansour MA, Jwaid AA, et al. Computed tomography-guided Tru-cut biopsy of lung mass, as an important diagnostic tool: Histopathological characteristics, age, sex distribution, and risk factors in Misurata Cancer Center, Libya. Asian J Oncol. 2017;3:111-115.
- Tuzi A, Bolzacchini E, Suter MB, Giaquinto A, Passaro A, et al. Biopsy and re-biopsy in lung cancer: the oncologist requests and the role of endobronchial ultrasounds transbronchial needle aspiration. J Thorac Dis. 2017;9:S405-S409.
- Jekunen AP. Role of Rebiopsy in Relapsed Non-Small Cell Lung Cancer for Directing Oncology Treatments. J Oncol. 2015;2015:1-11.
- Ilié M, Hofman P. Pros: Can tissue biopsy be replaced by liquid biopsy? Transl Lung Cancer Res. 2016;5:420-423.
- Esagian SM, Grigoriadou GΙ, Nikas IP, Boikou V, Sadow PM, et al. Comparison of liquid-based to tissue-based biopsy analysis by targeted next generation sequencing in advanced non-small cell lung cancer: a comprehensive systematic review. J Cancer Res Clin Oncol. 2020;146:2051-2066.
- Boskovic T, Stanic J, Pena-Karan S, Zarogoulidis P, Drevelegas K, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis. 2014;6:S99-S107.
- Boskovic T, Stojanovic M, Stanic J, Pena Karan S, Vujasinovic G, et al. Pneumothorax after transbronchial needle biopsy. J Thorac Dis. 2014;6:S427-S434.
- Covey AM, Gandhi R, Brody LA, Getrajdman G, Thaler HT, et al. Factors associated with pneumothorax and pneumothorax requiring treatment after percutaneous lung biopsy in 443 consecutive patients. J Vasc Interv Radiol. 2004;15:479-483.
- Khan MF, Straub R, Moghaddam SR, Maataoui A, Gurung J, et al. Variables affecting the risk of pneumothorax and intrapulmonalhemorrhage in CTguided transthoracic biopsy. Eur Radiol. 2008;18:1356-1363.
- Yeow KM, Su IH, Pan KT, Tsay PK, Lui KW, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004;126:748-754.
- Santoni-Rugiu E, Melchior LC, Urbanska EM, Jakobsen JN, Stricker K, et al. Intrinsic resistance to EGFR-Tyrosine Kinase Inhibitors in EGFR-Mutant Non-Small Cell Lung Cancer: Differences and Similarities with Acquired Resistance. Cancers. 2019;11:923.
- Stewart EL, Tan SZ, Liu G, Tsao MS. Known and putative mechanisms of resistance to EGFR targeted therapies in NSCLC patients with EGFR mutations-a review. Transl Lung Cancer Res. 2015;4:67-81.
- Leonetti A, Sharma S, Minari R, Perego P, Giovannetti E, et al. Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer. Br J Cancer. 2019;121:725-737.


Editors List
-
RAOUi Yasser
Senior Medical Physicist
-
Ahmed Hussien Alshewered
University of Basrah College of Medicine, Iraq
-
Sudhakar Tummala
Department of Electronics and Communication Engineering SRM University – AP, Andhra Pradesh
-
Alphonse Laya
Supervisor of Biochemistry Lab and PhD. students of Faculty of Science, Department of Chemistry and Department of Chemis
-
Fava Maria Giovanna
Google Scholar citation report
Citations : 558
Onkologia i Radioterapia received 558 citations as per Google Scholar report
Onkologia i Radioterapia peer review process verified at publons
Indexed In
- Directory of Open Access Journals
- Scimago
- SCOPUS
- EBSCO A-Z
- MIAR
- Euro Pub
- Google Scholar
- Medical Project Poland
- PUBMED
- Cancer Index
- Gdansk University of Technology, Ministry Points 20