Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 9
Evaluation of positioning accuracy and determination of the optimal margin for the planning target volume during radiation therapy on the Tomotherapy HD system
Tanzhas Shayakhmetov1*, Venera Bissengalyieva1, Yernar Orda1, Saniya Baiturova2, Daulet Berikbol2, Rauan Otynshiyev2, Aigul Brimova3, Bolat Saktashev3, Ainur Baissalbayeva2 and Ainur Samigatova32Radiation Oncology Department, UMIT International Oncological Center of Tomotherapy: Astana, Kazakhstan
3Clinical Department, UMIT International Oncological Center of Tomotherapy: Astana, Kazakhstan
Tanzhas Shayakhmetov, Medical Physics Department, UMIT International Oncological Center of Tomotherapy: Astana, Kazakhstan, Email: t.shayakhmetov@tomo.kz
Received: 28-Jul-2023, Manuscript No. OAR-23-108300; Accepted: 22-Aug-2023, Pre QC No. OAR-23-108300 (PQ); Editor assigned: 01-Aug-2023, Pre QC No. OAR-23-108300 (PQ); Reviewed: 08-Aug-2023, QC No. OAR-23-108300 (Q); Revised: 21-Aug-2023, Manuscript No. OAR-23-108300 (R); Published: 05-Sep-2023
Abstract
Relevance of research: The accurate positioning of patients during radiotherapy plays a crucial role in ensuring effective tumor control while minimizing the risk of overdosing normal tissues. The result of errors during patient’s setup may be target for underexposure of the cancer or overexposure of normal tissues. Therefore, Planning Target Volume (PTV) contains Clinical Target Volume (CTV) plus margin, which considers geometrical uncertainty due to organ motion, breathing and changing of patient position. Purpose of study: The purpose of this work is to calculate the margins using the van Herk formula and compare them with the values used in the International Oncological Center of Tomotherapy "UMIT". Methods: There were 212 patients in this investigation: 47 patients with brain tumors, 52 patients with pelvic tumors, 50 patients with breast cancer, 34 patients with head and neck cancer, 29 patients with esophageal cancer. The 5305 patient setup displacements were analyzed. The systematic and random errors were calculated for each case, and the optimal margins from CTV to PTV were calculated using the van Herk et al formula. Results: The results showed that in the case of the head and neck, brain, esophagus and pelvis the obtained values were within acceptable limits. The x and y offsets for the breast are outside the margins used in the clinic. Outcomes: In this work, the offsets from CTV to PTV were calculated and analyzed, taking into account systematic and random errors. The margins used in the clinic are sufficient for safe and high-quality radiation therapy. Exceeding values for the case of the breast may be due to respiration, which requires special monitoring and is the subject of further research. The use of IGRT and immobilization devices makes it possible to reduce dose delivery errors to the target, thereby increasing the safety of treatment.
Keywords
oncology, breast cancer, tumour, tomotherapy
Introduction
Accuracy of patient positioning is necessary condition for safe and high-quality radiation therapy. Image-guided Radiation Therapy (IGRT) is used in modern devices to reduce errors in dose delivery, it also makes possible to reduce geometric errors in patient positioning. The main sources of these errors are organ motion, impossibility of accurately tumor determination, limitation of visualization methods, incorrect patient setup [1]. The result of these errors may be target underexposure or normal tissues overexposure [2]. Therefore, Planning Target Volume (PTV) contains Clinical Target Volume (CTV) plus margin, which considers geometrical uncertainty due to organ motion, breathing and changing of patient position [2].
There are two types of errors during optimal margin determination in radiation therapy: random and systematic. These errors affect the dose differently. Systematic error is typical for one patient during the course of radiation therapy, it causes a shift of the entire planned dose distribution. Mostly, they occur due to decreasing of postoperative edema, tumor regression, weight loss and incorrect position of the patient during pre-radiation preparation. Error delineation is purely a systematic error and will equally affect to all stages of the treatment process. Random errors cause blurring of the dose distribution. They occur due to daily changes of organ movements, as well as improper positioning of the patient [1].
A complete characterization of all geometric uncertainties should lead to an objective choice of CTV to PTV margins. Using the van Herk formula it is possible to calculate the offsets from CTV to PTV, taking into account systematic and random errors [3].
The purpose of this work is to calculate the margins using the van Herk formula and compare them with the values used in the International Oncological Center of Tomotherapy "UMIT".
Methods and Materials
A total of 212 patients were investigated. All patients were treated with TomoTherapy HD Accuray Inc™ radiotherapy system. The distribution of patients was 47 with brain tumors, 52 pelvic cancer patients, 50 breast cancer patients, 34 patients with H&N tumors and 29 patients with esophageal cancer.
CT simulation/dosimetric planning
Patients with brain tumors were immobilized with 3-point thermoplastic mask using head rest and knee rest. Slice thickness was 2 mm Lead marks were located on the frontal part of the head.
Patients with H&N tumors were immobilized with 5-point thermoplastic mask, using head rest, ‘bite lock’ for tongue fixation, knee rest. Slice thickness was 2 mm-3 mm. Lead marks were located on the chin.
Patients with breast and esophageal cancer were immobilized with 6-point thermoplastic mask, using “breast board” and knee rest. Hands were positioned over head. If the target was in the upper part of the esophagus, a 5-point mask was used. Slice thickness 3 mm.
Pelvic cancer patients were immobilized with 5-point thermoplastic mask, using head rest, ‘bite lock’ for tongue fixation, knee rest. Patients drunk 4 cups of water 30 minutes before scanning for bladder filling. Lead marks were located in the region of the iliac bones. Slice thickness 3 mm.
CT images were imported to MIM Maestro software for target and normal tissue delineation. The following CTV to PTV margins were used: 5 mm for brain, 5 mm for H&N, 10 mm for esophagus, 7 mm for breast, 10 mm for pelvis
Acquired images with target and organs at risk contours were imported to the TomoTherapy Planning Station.
Igrt
TomoTherapy HD system combines IMRT and IGRT. The feature of this system is opportunity of everyday megavoltage CT scanning with maximum energy 3,5 MeV [4]. Three scanning regimes are available: coarse (3 mm and 6 mm), normal (4 mm), fine (2 mm) [5].
Image matching using MVCT data is done online. Daily correction of the patient's position before treatment makes it possible to correct both random and systematic error components, thereby increasing the accuracy of radiotherapy.
Scanning protocol
Before a radiation therapy treatment, patients were placed on the couch and fixed with appropriate immobilization devices.
Scanning for MVCT and registration of displacements are carried out daily. Displacements are recorded in the transversal, coronal and sagittal planes.
Scanning is carried out in the coarse mode (3 mm or 6 mm) and includes the PTV zone. For the pelvic cancer patients, the scanning area included the PTV and the full bladder.
Data Analysis
There were 3675 x, y, z displacement values of patients with brain tumors; 3723 for the pelvis; 3633 for breast cancer; 2778 for the head and neck cancer; 2106 for the esophagus collected.
Patients are grouped by location to analyze systematic and random errors.
The calculation of the CTV to PTV margins for a particular localization was performed using the van Herck formula. Van Herk et al. analytically developed a formula to calculate the margin from CTV to PTV that provides the minimum dose at 95% CTV for 90% of patients.

where Σ-systematic error, σ -random error
Results
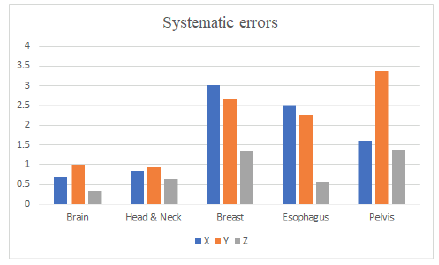
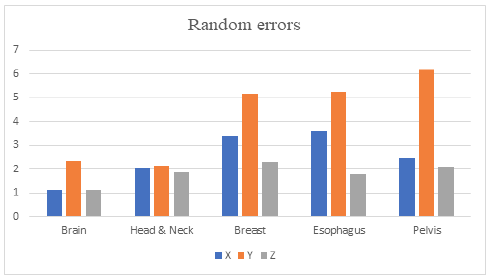
In this investigation 1225 brain, 926 H&N, 1211 breast, 702 esophagus, 1241 pelvis patient’s setup were analyzed. Systematic and random errors for each plane and localization were calculated (Table 1 and Figure 1).
Tab.1. Systematic and random errors for each direction and localization
|
|
Brain | Head & Neck | Breast | Esophagus | Pelvis | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
X |
0,68 | 1,11 | 0,84 | 2,01 | 3,02 | 3,39 | 2,50 | 3,61 | 1,60 | 2,46 |
|
Y |
1,00 | 2,33 | 0,93 | 2,14 | 2,65 | 5,15 | 2,25 | 5,25 | 3,38 | 6,17 |
|
Z |
0,33 | 1,11 | 0,64 | 1,88 | 1,36 | 2,30 | 0,58 | 1,78 | 1,38 | 2,12 |
Figure 1: Systematic errors distribution
Systematic errors vary from 0,68 mm to 3,38 mm. Random errors vary from 1.11 mm to 6.17 mm.
The maximum systematic errors were observed in the case of the pelvis along the y axis, along the x and z axes - for the breast.
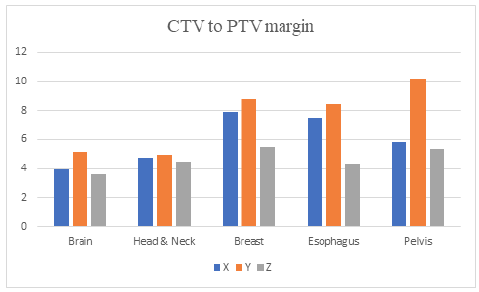
The CTV to PTV margins for each localization and axes were calculated using van Herk equation (Table 2 and Figure 2).
Tab.2. Calculated CTV to PTV margins for each direction and localizations.
|
|
Brain | Head & Neck | Breast | Esophagus | Pelvis |
|---|---|---|---|---|---|
|
X |
3,96 | 4,74 | 7,90 | 7,53 | 5,82 |
|
Y |
5,14 | 4,92 | 8,76 | 8,42 | 10,20 |
|
Z |
3,60 | 4,46 | 5,47 | 4,33 | 5,37 |
Figure 2: Random errors distribution
The maximum margin along x axis is observed for breast –7.9 mm, the minimum is for brain – 3.96 mm.
The maximum margin along y axis is observed for pelvis – 10.2 mm, the minimum is for H&N – 4.92 mm.
The maximum margin along z axis is observed for breast – 5.47 mm, the minimum is for brain – 4.92 mm.
The most identical displacements along all axes are observed for the H&N cancer patients (Figure 3).
Figure 3: CTV to PTV margins distibution
Discussion
Daily MVCT makes possible to analyze systematic and random setup errors. Properly selected margins prevent shifting of the dose distribution, thus it is possible to irradiate the target as much as possible, while minimizing dose to healthy organs.
The following CTV to PTV margins are used in our clinic: 5 mm for brain, 5 mm for H&N, 1 cm for the esophagus, 7 mm for breast, 10 mm for pelvis in all directions. The margins which is used in our clinic were compared with the values calculated in this study for the brain, OG&N, esophagus, and small pelvis. The x and y offsets for the breast are outside the margins used in the clinic. Possible reasons for such discrepancies are the patient's breathing, insufficient fixation rigidity, sample size, positioning and mobilization devices, etc.
It has also been noted that fittings in patients with large breasts are likely to have large errors because the soft tissues of the breasts are highly deformable and movable. Because the breast is not a rigid structure, deformation or movement of fat or relaxation of muscles may be more significant in patients with large breasts, resulting in large setup errors [6].
The obtained results make it possible to verify the correct choice of the margin from CTV to PTV. The margins used in the clinic in conjunction with the immobilization devices will keep the geometric errors within acceptable limits. This fact can be used in cases where MVCT is not possible for a number of reasons or to reduce the number of MVCTs, thereby reducing the treatment time, which is especially important during a period of high volume of patients [3].
Conclusion
In this work, the offsets from CTV to PTV were calculated and analyzed, taking into account systematic and random errors. The margins used in the clinic are sufficient for safe and high-quality radiation therapy. Exceeding values for the case of the breast may be due to respiration, which requires special monitoring and is the subject of further research. The use of IGRT and immobilization devices makes it possible to reduce dose delivery errors to the target, thereby increasing the safety of treatment.
The use of the van Herk formula makes it possible to reduce the margin from CTV to PTV, thus reducing the dose on healthy organs and tissues. Although margin reduction is a potential strategy, it demands utmost caution and necessitates the utilization of image-guided radiation therapy for optimal precision and safety.
References
- Van Herk M Errors and margins in radiotherapy Seminars in Radiation Oncology 2004:14;52-64.[Google Scholar] [Crossref]
- Molana S, Arbabi F, Sanei M, Hashemi E, Tajvidi M, et al. Evaluation of patient setup accuracy and determination of optimal setup margin for external beam radiation therapy using electronic portal imaging device. Cancer Ther. Oncol. Int. J., 2018;11:48-55. [Google Scholar] [Crossref]
- Van Herk M, Remeijer P, Rasch C, Lebesque JV. The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int. J. Radiat. Oncol.* Biol.* Phys. 2000;47:1121-1135. [Google Scholar] [Crossref]
- Langen KM, Papanikolaou N, Balog J, Crilly R, Followill D, el al. QA for helical tomotherapy: report of the AAPM task group 148 a. Med. phys. 2010;37:4817-4853. [Google Scholar] [Crossref]
- Thondykandy BA, Swamidas JV, Agarwal J, Gupta T, Laskar SG et al. Setup error analysis in helical tomotherapy based image-guided radiation therapy treatments. J. Med. Phys./Assoc. Med. Phys. India. 2015;40:233.[Google Scholar] [Crossref]
- Seppälä J, Vuolukka K, Virén T, Heikkilä J, Honkanen JT, et al. Breast deformation during the course of radiotherapy: The need for an additional outer margin. Phys. Med. 2019;65:1-5.[Google Scholar] [Crossref]