Research Article - Onkologia i Radioterapia ( 2020) Volume 14, Issue 4
Evaluation of ocular comorbidities among cataract surgery through medical imaging method
Afshan Sharghi1, Habib Ojaghi2*, Telma Zahirian Moghadam3, Arezoo Ranjbar4 and Mehdi Ranjbar42Department of Surgery, School of Medicine and Allied Medical Sciences,Imam Reza Hospital, Ardabil University of Medical Sciences, Ardabil, Iran
3Social Determinations of Health Research Centre, Ardabil University of Medical Sciences, Ardabil, Iran
4Medical School, Ardabil University of Medical Sciences, Ardabil, Iran
Habib Ojaghi, Department of Surgery, School of Medicine and Allied Medical Sciences,Imam Reza Hospital, Ardabil University of Medical Sciences, Ardabil, Iran, Email: habibojaghi@yahoo.com
Received: 19-Jan-2020 Accepted: 26-Aug-2020 Published: 15-Sep-2020
Abstract
Introduction and Objective: Imaging plays an indispensable role in clinical care in ophthalmology, ranging from diagnostics to risk stratification and treatment monitoring. Imaging biomarkers were identified in many diseases such as diabetic retinopathy, age-related macular degeneration and glaucoma. Cataract is the most common cause of blindness in the world and it is estimated that about one hundred thousand cases of cataract surgery are performed in Iran annually. One of the factors affecting cataract is ocular comorbidities. Due to the rarity of studies in this field, this study aimed to evaluate the ocular complications of comorbidities in patients undergoing cataract surgery at Noor Surgery Centre in Ardabil, Iran.
Materials and Methods: This descriptive cross-sectional study was performed on 780 patients referred to Noor Ophthalmology Clinic in Ardabil city with cataract diagnosis. Data were collected by a researcher using a checklist. Data analysis was performed by SPSS 25 software using descriptive statistics
Results: Of the 1018 eyes studied, 590 (58%) were female and 428 (42%) were male. Mean age of patients was 65.88 ± 11.43 years. The mean intensities of PSC, Nuclear, and cortical cataracts were 4.56 ± 0.62, 4.79 ± 0.89, and 4.21 ± 0.48, respectively. Our findings revealed a significant association of cataract type in diabetic patients with normal retina (p=0.034), pseudoexfoliation syndrome (p=0.001), hyperopia (p=0.008), corneal opacity (p=0.036) and nasolacrimal duct obstruction (p=0.032) in compare with other patients. There was no significant difference in other comorbidities in terms of cataract types.
Conclusions: Since age, sex and comorbidity factors can affect cataract, periodic medical examinations and training in healthy lifestyle can be an effective step in preventing or decreasing cataracts formation, as well as improvement of prognosis of cataract surgery through OCT angiography.
Keywords
Medical imaging, ocular angiography, cataract, morphology, diabetic retinopathy, glaucoma, comorbidities, Magnetic Resonance Imaging (MRI), intraocular lens
Abbrevations
NPDR: Non-Proliferative Diabetic Retinopathy; PDR: Proliferative Diabetic Retinopathy; CSME: Clinically Significant Macular Edema; PEX: Pseudoexfoliation Syndrome; TBX: Trabeculectomy; PI: Peripheral Iridectomy; AMD: Age Related Macular Degeneration; GA: Geographic Atrophy; IV: Intra- Vitreal; NLDO: Nasolacrimal Duct Obstruction; DCR: Dacryocystorhinostomy
Introduction
Ophthalmologists perform a wide array of interventions on the orbital contents. The surgical treatment of glaucoma, cataracts, retinal detachment, and ocular trauma or malignancy results in alteration of the standard anatomy, which is often readily evident at radiologic examinations. Although knowledge of patients’ surgical history is helpful, this information is often not available at the time of interpretation. Fortunately, there are characteristic posttreatment findings that enable diagnosis. The imaging features of the most commonly performed ophthalmologic procedures are highlighted, with emphasis on computed tomography and Magnetic Resonance Imaging (MRI), because they are currently the primary modalities involved in evaluating the orbits. Computed Tomography (CT) and MR imaging are the two most frequently used modalities (Figure 1).
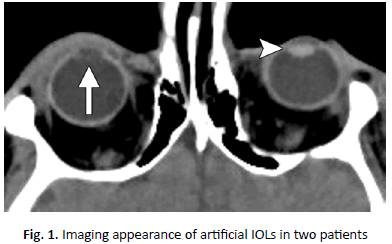
Figure 1. Imaging appearance of artificial IOLs in two patients
A cataract is the opacity of the lens in the eye that is considered as one of the major causes of blindness worldwide and its only treatment is surgery [1]. Cataract surgery is one of the most common types of surgeries in ophthalmology and has gradually become more precise and less invasive [1,2]. This opacity is caused by the absorption of water, glucose or protein by different lens layers [3,4]. Various factors, such as aging, UV exposure, long-term use of certain medications, systemic diseases, trauma, skin diseases such as eczema and lupus, are associated with this disease [5,7]. The World Health Organization estimates the number of people with cataracts to be 95 million in 2014. Various studies have shown that the incidence of cataract increases from 3.9% at 55-64 years to 92.6% at 80 years of age. In addition, the presence of cataracts has been linked to increased mortality, which may be due to the association between cataracts and systemic diseases such as type 2 diabetes or smoking [8,9]. Over the past two decades, the incidence of cataract-induced blindness has been decreasing as the cataract surgery rate, which means the number of annual surgeries/1000000 population, has been increasing due to improvements in surgical techniques and technologies. However, cataract remains the leading cause of blindness in middle and low income countries, which accounts for 50% of blindness in these areas, while cataract is responsible for only 5% of blindness in developed countries. Therefore, implementation of a set of strategies is needed to improve access to medical services and to provide ocular screening and the appropriate quality of treatment for these patients in developing countries [10]. The epidemiology of cataracts in Iran is unclear. In a cross-sectional study conducted in 22 districts of Tehran, cataract was the most common visual disorder with a relative prevalence of 36%. According to another study conducted on residents of Tehran aged 40 years or older, cataract have been reported in one fifth of the population over 40 years. The prevalence rate in females is 24.5% and in males about 22.1%. In both sexes the incidence has increased with age. Overall, about 5.3% of people had either low vision patients or blindness because of the disease. Cataract surgery for one million people per year, or CSR, is one of the World Health Organization's guidelines for control of cataract-induced visual dysfunction and blindness. According to studies in Iran, this index has increased significantly from 526 in 2000 to 1331 in 2005; however, it is lower than the WHO recommendation [11] (Figure 2).
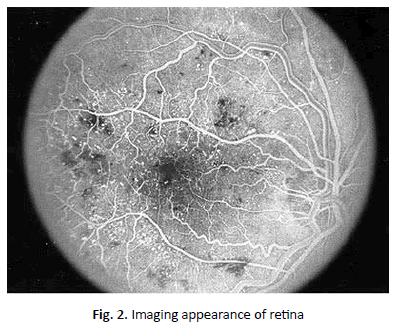
Figure 2. Imaging appearance of retina
Generally, cataracts are divided into several categories:
• Primary cataract: This type of cataract is the age-related type that is the most common type of cataract and its prevalence is directly related to age
• Secondary cataract: This type of cataract may be occurred due to the underlying disease such as surgery due to other eye diseases (e.g., glaucoma), intraocular cancers, diabetes, long-term use of some drugs (e.g., corticosteroid) and X-ray m
• Congenital cataract: This type of cataract is seen in children and may be hereditary or may be related to some congenital anomalies. In some cases, it occurs without a clear cause
• Traumatic cataract: This type of cataract is directly related to the history of eye trauma and may occur immediately after trauma or even years later [12,13]. Few studies have been conducted in this area. Due to the impact of comorbidities on cataract, this study was performed to evaluate the ocular complications of comorbid diseases in patients undergoing cataract surgery Noor Surgery Centre, Ardabil, Iran during 2018
Material and Method
The present cross-sectional study was performed on 780 patients (1018 eyes) undergoing cataract surgery at Noor Ophthalmology Clinic from January to December 2018. Exclusion criteria included patients under 18 years of age, previous corneal surgery and previous eye trauma. In all patients, preoperative ophthalmic examination including slit lamp examination, tonometry, visual acuity and indirect funduscopic with dilated pupils were performed. Cataract severity measurements were performed using the LOCS 3 (Lens Opacities Classification System, Version 3) system, obtained by comparing the patient's lens shape with the classification image (Figure 3), a reliable and widely used method in scientific research fields [14]. Patient information was then recorded in the checklist. The collected data were analysed using descriptive statistics, mean, standard deviation, frequency and percentage. SPSS software version 25 was applied for data analysis.
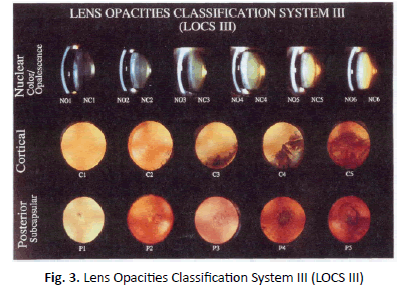
Figure 3: Lens Opacities Classification System III (LOCS III)
All standards are the boundaries of the scaling intervals. There are no standards or degrees of zero in LOCS III. Indeterminate interval of image is assigned by the scorer: The clouding intensity should be greater than the lower standard intensity and less than or equal to the higher standard intensity. Each interval is assumed to be divided into 10 equal sections between the reference standards, each of which is 0.1 unit of interval. For each type of cataract, or for NC, higher ratings indicate greater severity. The scale ranges from 0.1 (transparent or colourless) to 5.9 (very blurry [regarding to C and P]) or 6.9 (very blurry or tanned [in NO and NC cases). Then, a decimal degree is assigned to each clouding using 0.1-unit intervals. The decimal point should indicate the unknown position in the standard range. For example, a grade of 2.5 means that the cataract severity is judged to be between standard 2 and 3. If the cataract intensity is equivalent to the standard image intensity of 3, it is 3.0. If the value is obtained to be less than the intensity shown in Figure 1, but is greater than the midpoint, the score is in the range of 2.6 to 2.9. Similarly, a score of 1.1 to 2.0 is assigned if the cataract is greater than standard with score 1 but less than or equal to the intensity shown in standard with score 2. The most severe cataracts shown in the reference standards are 5 for C, P, and 6 for NC and NO, respectively. The highest scores for each are 5.9 and 6.9, respectively. Therefore, the assigned score ranges from 0.1 to 5.9 or 6.9 [14].
Grading of corneal clouding in patients was performed according to the study of Couprie et al. grade 1: no corneal clouding visible; grade 2: mild corneal clouding can be observed, but it is possible to observe visibility of details of the anterior chamber, iris and retina; grade 3: moderate corneal clouding is obvious, with partial masking of anterior chamber, iris details and loss of fundus view; grade 4: this grading is characterized by severe corneal clouding and anterior chamber and posterior segment of the eye is not visible [15]. The classification of diabetic retinopathy is given in (Table 1) [16].
| Findings Observable on Dilated Ophthalmoscopy | Proposed Disease Severity Level |
|---|---|
| No abnormalities | No apparent retinopathy |
| Microaneurysms only | Mild nonproliferative diabetic retinopathy |
| More than just microaneurysms but less than severe nonproliferative diabetic retinopathy | Moderate nonproliferative diabetic retinopathy |
| Any of the following: more than 20 intraretinal hemorrhages in each of 4 quadrants; definite venous beading in 2+ quadrants; Prominent intraretinal microvascular abnormalities in 1+ quadrants And no signs of proliferative retinopathy | Severenonproliferative diabetic retinopathy |
| One or more of the following: neovascularization, vitreous/preretinal hemorrhage |
Proliferative diabetic retinopathy |
Table 1. Classification of diabetic retinopathy
Results
In this study, a total of 1018 eyes of 780 patients were studied, of whom 445 (57.1%) were female and 335 (42.9%) were male. Of the 1018 eyes studied, 590 (58%) belonged to females. Mean age of patients was 65.88 ± 11.43 years and mean age of female and male patients was 65.05 ± 10.93 years and 66.98 ± 11.99 years, respectively. Figure 2 shows age group distribution of patients. In terms of distribution of the involved eye, 238 patients (30.5%) had involvement in both eyes, followed by 292 patients (37.4%) with right eye only, and 250 patients (32.1%) only the left eye. Overall, involvement was 530 (52.1%) in the right eye, and 488 (47.9%) in the left eye (Figure 4).
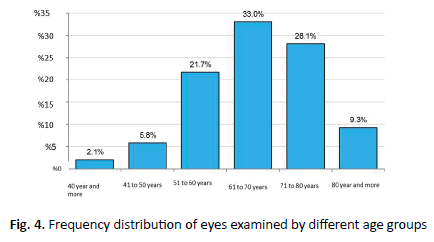
Figure 4. Frequency distribution of eyes examined by different age groups
Frequency Distribution of Comorbidities in Studied Patients
Table 2 shows the frequency of comorbidities in patients, with the following results. According to Table 2, diabetic patients were divided into two groups of normal (no retinal involvement 56 patients, 7.2%) and diabetic retinopathy (53 patients, 6.8%). Given that some people had bilateral PEX, of the 64 patients with PEX, 98 eyes (9.6%) developed PEX, 88 (8.6%) (had normal ocular pressure (Mean 17.65 ± 3.41) and 10 eyes (0.98%) had high ocular pressure (mean 23.95 ± 5.94), which received drug treatment. Furthermore, 17 (2.2%) of all patients exhibited mean ocular pressure (25.54 ± 4.03 mmHg) ranged from 21 mm to 35 mm Hg. They were unaware of their ocular pressure and has not been under any intraocular pressure-lowering treatments. Of all patients, 19 (22.49 ± 4.27 mmHg) were treated with one glaucoma drop followed by 9 (18.67 ± 4.87 mmHg) treated with two drops of glaucoma, 12 patients (19.5 ± 5.76 mmHg) with three drops of glaucoma, and 1 person (ocular pressure: 18 mmHg) treated with four drops of glaucoma. Moreover, 19 patients (2.4% of patients: 21 eyes [2.1% of total eyes]) had unilateral corneal clouding and 2 patients had bilateral clouding. Of these, 7 showed grade II, followed by Grade III (11 cases), and Grade IV (1 cases).
| Disease | Frequency (%) | |
|---|---|---|
| Diabetes with normal retina | 56 (2/7) | |
| Diabetic Retinopathy | Mild NPDR | 31 (9/3) |
| Moderate NPDR | 13 (7/1) | |
| Sever NPDR | 0 | |
| Very Sever NPDR | 0 | |
| Early PDR | 0 | |
| High Risk PDR | 2 (3/0) | |
| Sever PDR | 0 | |
| Regressed PDR | 4 (5/0) | |
| CSME | 3 (4/0) | |
| total | 53 (8/6) | |
| PEX | Unilateral | 30 (8/3) |
| Bilateral | 34 (4/4) | |
| total | 64 (2/8) | |
| High eye pressure | 17 (2/2) | |
| History of glaucoma medication | Treated with 1 drop | 19 (4/2) |
| Treated with 2 drop | 9 (2/1) | |
| Treated with 3 drop | 12 (5/1) | |
| Treated with 4 drop | 1 (1/0) | |
| History of glaucoma surgery | TBX | 5 (6/0) |
| PI | 1 (1/0) | |
| total | 6 (8/0) | |
| pterygium | With surgery history | 6 (75/0) |
| Without surgery history | 6 (75/0) | |
| total | 12 (5/1) | |
| Lasik history | 2 (3/0) | |
| Dry Eye | 5 (6/0) | |
| One Eye | 18 (3/2) | |
| Hypertensive Retinopathy | 1 (1/0) | |
| History of RD surgery | 1 (1/0) | |
| AMD | Unilateral Dry | 2 (3/0) |
| Bilateral Dry | 4 (5/0) | |
| Unilateral GA | 1 (1/0) | |
| Bilateral GA | 0 | |
| Unilateral wet | 0 | |
| Bilateral wet | 4 (5/0) | |
| History of one IV injection | 1 (1/0) | |
| History of two IV injections | 0 | |
| History of three injections | 0 | |
| total | 11 (4/1) | |
| Ptosis | Right eye | 1 (13/0) |
| Left eye | 1 (13/0) | |
| Bilateral eye | 1 (13/0) | |
| total | 3 (39/0) | |
| Corneal opacity | Grade I | 0 |
| Grade II | 7 (9/0) | |
| Grade III | 11 (4/1) | |
| Grade IV | 1 (1/0) | |
| total | 19 (4/2) | |
| NLDO | Tearing | 5 (64/0) |
| Purulent discharge | 0 | |
| History of probing | 0 | |
| DCR History | 8 (03/1 ) | |
| Total | 13 (67/1 ) | |
| Optic nerve atrophy | Mild | 5 (64/0) |
| Moderate | 5 (64/0) | |
| Severe | 4 (51/0) | |
| Total | 14 (79/1) | |
| Hyperopia | 20 (6/2) | |
| Myopia | 60 (7/7 ) | |
Table 2. Comorbidity frequency of patients
Twenty patients (2.6%) had hypermetropia (mean 3.43 ± 2.58 diopters and range from 1 to 11.12 diopters). Sixty patients (7.7%) had myopia (a mean of -11.05 ± 5.38 diopters and a range of -1 to -22.5 diopters. There was a significant difference between diabetic patients with normal retina and other patients in terms of cataract types (p=0.034). In these patients, posterior sub capsular cataract was the most type of cataract. No significant difference was found between diabetic patients with retinopathy and other patients in terms of cataract types (p=0.133). There was a significant difference between patients with pseudo exfoliation syndrome and other patients in terms of cataract types (p=0.001). Nuclear cataracts were more common in these patients as compared to other patients.
There was no significant difference between patients with myopia (p=0.140), age related macular degeneration (p=0.065), optic nerve atrophy (p=0.081), patients with pterygium (p=0.292), ocular hypertension (p=0.0874) and other patients in terms of cataract types (p=0. 140). There was a significant difference between patients with hypermetropia and other patients in terms of cataract types (p=0.008). Posterior sub-capsular cataract was more common in these patients. Our results demonstrated a significant difference between patients with corneal clouding and other patients in terms of cataract types (p=0.036). In these subjects, posterior sub-capsular cataracts and nuclear cataracts were found to be more common. Our data exhibited a significant difference between patients with nasolacrimal duct obstruction and other patients in terms of cataract types (p=0.032), which posterior sub-capsular cataract was more common in these patients. In addition, no significant difference between patients with pterygium and other patients in terms of cataract types (p=0.292). Table 3 shows the frequency of different types of comorbidities in the studied patients based on the age group.
| Disease age | Diabetic with | Other patients | Myopia | Other patients | PEX | Other patients |
|---|---|---|---|---|---|---|
| Less than 40 years | 0 | 21 (2/2%) | 0 | 21 (2/2%) | 0 | 21 (2/2%) |
| 41-50 years | 4 (1/7%) | 55 (7/5%) | 8 (3/13%) | 51 (3/5%) | 2 (1/3%) | 57 (0/6%) |
| 51-60 years | 18 (1/32%) | 203 (1/21%) | 27 (0/45%) | 194 (3/20%) | 8 (5/12%) | 213 (3/22%) |
| 61-70 years | 26 (4/46%) | 310 (2/32%) | 20 (3/33%) | 316 (0/33%) | 9 (1/14%) | 327 (3/34%) |
| 71-80 years | 8 (3/14%) | 278 (9/28%) | 1 (7/1%) | 285 (7/29%) | 29 (3/45%) | 257 (9/26%) |
| More than 80 years | 0 | 95 (9/9%) | 4 (7/6%) | 91 (5/9%) | 16 (0/25%) | 79 (3/8%) |
| Total | 56 | 962 | 60 | 958 | 64 | 954 |
| p-Value | 001/0 | <001/0 | <001/0 | |||
Table 3. Frequency of associated diseases by age group
The highest prevalence of myopia (45%) was observed in the age group of 51-60 years (Figure 5).
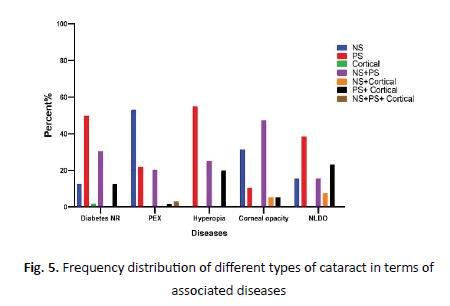
Figure 5: Frequency distribution of different types of cataract in terms of associated diseases
Highest prevalence of diabetes with normal retina (46.4%), diabetic retinopathy (46%), hyperopia (40%), corneal opacity (36.8%), and NLDO (46.2%) was found in the age group of 61-70 years. Furthermore, the highest prevalence of PEX (45.3%), AMD (45.5%), and pterygium (58.3%) were in the age group of 71-80 years. Moreover, the highest prevalence of ocular hypertension (29.4%) and optic nerve atrophy (28.6%) were seen in the age groups 61-70 and 71-80 years, respectively. A statistically significant relationship was found between age group of diabetic patients with normal retina (p=0.001), PEX (p<0.001), and myopia (p<0.001), but no significant relationship was determined between age group and other diseases.
Discussion
The goal of cataract surgery is to achieve the best post-operative results and restore visual acuity; numerous factors such as age, gender and comorbidities have a significant impact on postoperative visual acuity. In this study a total of 1018 eyes of 780 patients were enrolled. The findings of the present study showed a higher percentage of women suffered from cataract (female to male ratio: 1.3 fold). Similar findings were found by previous studies, where higher cataract surgery has been performed for women female-to-male ratio: 1.2-fold to 1.8- fold), [17-23]; however, in some studies, the ratio of men and women has been reported to be the same [24,25]. The mean age of our study population was 65.88 ± 11.43 years compared with the mean age of cataract surgery patients in more advanced countries, indicating involvement of younger people with this disease in our area. For example, the mean ages of patients undergoing cataract surgery in the United Kingdom (78.84 ± 7.01 years) [17], Ireland (75.2 ± 10.57 years) Argentina (71.9 ± 9.6 years) [18], Lithuania (71.68 ± 9.77 years) [19], and Portugal (69 ± 10 years) [20,21] are higher than our study.
But the mean age of these patients in Nepal and India has been reported to be lower as compared to the present study [22-24]. In Iran, the mean age of patients undergoing cataract surgery in Yazd was 69.5 years [25], which is higher than the present study. In Tehran, this mean (64.92 ± 11.48 years) was similar to the present study. In addition to racial differences, differences in living conditions in terms of sunlight, quality of life and better health care and preventive care in more developed countries can contribute to this age difference. In the present study, 32.3% of all cataract surgery candidates had at least one comorbid disease. So far, few studies have examined ophthalmic comorbidities in patients undergoing cataract surgery, and little is known about this. Day et al. study in the United Kingdom [17] showed that 36% of patients undergoing cataract surgery had at least one eye disease. This rate was reported in Lithuania (48.6%), China (34.1%) (34%), and Australia (36%) [26,27], indicating a relatively lower prevalence of ocular comorbidities in patients undergoing cataract surgery in our study. As the prevalence of ophthalmic diseases (e.g., pseudo exfoliation syndrome, diabetic retinopathy, glaucoma and age-related macular degeneration) increases by age. This age difference between studies may be the main reason for the lower prevalence of ocular comorbidities in the present study. For instance, the mean age of our study population was 65.88 ± 11.43 years, while the mean age of patients in the United Kingdom was reported to be 78.84 ± 7.01 years, followed by 71.68 ± 9.77 years in Lithuania, 69.4 ± 10.5 years in China and 74.6 ± 7.2 years in Australia.
The most common ocular comorbidities observed in patients undergoing cataract surgery in the present study were pseudo exfoliation syndrome (8.2%), diabetic retinopathy (6.8%), and glaucoma (4.2%). The most common ocular comorbidities in the UK are age-related macular degeneration (9.8%), glaucoma (9.2%), and diabetic retinopathy (4.1%) as reported by Day et al. [17]. Varoniukait et al. reported that glaucoma (31.3%), agerelated macular degeneration (10.8%), and diabetic retinopathy (4.8%) were the most common ocular comorbidities [19]. Liu et al. in China showed that glaucoma (19.4%), retinal disorders (19.4%), and diabetic retinopathy (8.3%) were the most common ocular diseases [26] another study by Pham et al. in Australia indicated that age-related macular degeneration (12.6%), glaucoma (10.6%), and diabetic retinopathy (9%) were the most prevalent ocular comorbidities [27]. Diabetic retinopathy and glaucoma are common in all studies of patients undergoing cataract surgery, but age-related macular degeneration, which has been prevalent in other studies, is less prevalent in the present study. This may be due to the lower mean age of the patients evaluated in this study.
Present study showed a significant association of cataract type with normal retina diabetic (p=0.034), pseudo exfoliation syndrome (p=0.001), hyperopia (p=0.008), corneal opacity (p=0.036), nasolacrimal duct obstruction (p=0.032), in compare with other patients. So that diabetic patients with normal retina had PSC more than other patients whereas NS type cataract was lower (12.5% vs. 28.9%); in patients with PEX NS type, cataract was found to be higher than other patients (53.1% vs. 26.3%). In patients with hyperopia, cataract type PS was higher as compared to other patients (55% vs. 37.1%), mixed NS+PS type cataracts (47.4% vs. 26.2%) were higher in patients with corneal opacity than other patients and mixed PS+Cortical type cataract was higher in patients with nasolacrimal duct obstruction in comparison with other patients (23.1% vs 5.1%). Other studies have not included such evaluation.
In this study we also investigated the prevalence of comorbidities by age group of patients. The results revealed a significant statistical relationship between age group of patients with diabetic patients with normal retina (p=0.001), PEX (p<0.001) and myopia (p<0.001). So that the most prevalence of myopia was in the age group of 51-60 years. The highest prevalence of diabetes with normal retina was found in the age group of 61-70 years; and the highest prevalence of PEX was in the age group of 71-80 years. Varoniukait et al. in Lithuania19] showed a significant statistical difference between the age groups in terms of glaucoma and AMD. As a result, glaucoma cases were higher in 71-80 years of age, whereas AMD was highest in both groups of 71 to 80 and over 81 years which is consistent with our study and given the high prevalence of the above-mentioned diseases in older ages, it is justifiable.
Conclusion
Imaging of the eye is an integral part of ophthalmic examination, and is also essential for the diagnosis, assessment of severity and progression, and evaluation of management of ocular disease. Advances in imaging technology are progressing at a rapid pace. A number of aspects of optical imaging including the role of Optical Coherence Tomography (OCT) in corneal and refractive surgery, optimal imaging of the eye during toric Intraocular Lens (IOLs) implantation, and the role of aberrometry during anterior segment imaging. Cataract extraction with implantation of an artificial Intraocular Lens (IOL) implant is the currently accepted treatment for symptomatic cataracts, other than the situations delineated in the previous section. Although there are several different designs that are commercially available, the basic components of an IOL implant include the central optic portion and two haptics that hold the device in position. Highresolution, high-field MRI scans may become an important tool for imaging the structures of the eye and retina, since conventional imaging methods like ultrasound imaging, partial coherence interferometry, and optical coherence tomography are limited by optical distortions or depth visualization, and have limited penetration through ocular structures such as the iris and sclera. MRI provides depth visualization of the entire eye in any desired anatomic plane. Moreover, MRI does not obstruct binocular vision and enables research of accommodating structures of the eye. Our study showed that age, sex, and comorbidity factors can affect cataract, and the differences observed in different studies can be associated with various causes, including differences in sample size, sex distribution, and age, differences in the inclusion criteria, differences in ethnic, genetic, and environmental factors. Of course, awareness of this discrepancy in the data may provide more information about the specific population of Ardabil for our cataract surgeons in our region.
Acknowledgment
This article is taken from the student thesis at Ardabil University of Medical Sciences and has a code of ethics, ARUMS. REC 1397.148.
References
- Chen W, Zuo C, Chen C, Su J, Luo L, et al. Prevalence of corneal astigmatism before cataract surgery in Chinese patients. J Cataract Refract Surg. 2013;39:188-192.
- Hoffmann PC, Auel S, Hütz WW, JJo C, Surgery R. Results of higher power toric intraocular lens implantation. J Cataract Refract Surg. 2011;37:1411-1418.
- Mohammadi M, Naderan M, Pahlevani R, Jahanrad A. Prevalence of corneal astigmatism before cataract surgery. Intern Ophthalmol. 2016;36:807-817.
- Khan MI, Muhtaseb MC, Surgery R. Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. J Cataract Refract Surg. 2011;37:1751-1755.
- Thompson J, Lakhani N. Cataracts. Prim Care. 2015;42:409-423.
- Liu YC, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. Lancet. 2017;390:600-612.
- Vinson JA. Oxidative stress in cataracts. Pathophysiol. 2006;13:151-162.
- Rao GN, Khanna R, Payal A. The global burden of cataract. Curr Opin Ophthalmol. 2011;22:4-9.
- Abraham AG, Condon NG, Gower EW. The new epidemiology of cataract. Ophthalmol Clin North Am. 2006;19:415-425.
- Khanna R, Pujari S, Sangwan V. Cataract surgery in developing countries. Curr Opin Ophthalmol. 2011;22:10-14.
- Ashrafi E, Alipor F. Distribution of cataract and its causes. Ophthal Nur. 2012;1:7-8.
- Marcos S, Rosales P, Llorente L, Jiménez-Alfaro I. Change in corneal aberrations after cataract surgery with 2 types of aspherical intraocular lenses. J Cataract Refract Surg. 2007;33:217-226.
- Memon AF, Mahar PS, Memon MS, Mumtaz SN, Shaikh SA. Age-related cataract and its types in patients with and without type 2 diabetes mellitus: a hospital-based comparative study. J Pak Med Assoc. 2016;66:1272-1276.
- Chylack LT, Wolfe JK, Singer DM, Leske MC, Bullimore MA, et al. The lens opacities classification system III. Arch Ophthalmol. 1993;111:831-836.
- Wasielica-Poslednik J, Politino G, Schmidtmann I, Lorenz K, Bell K, et al. Influence of corneal opacity on intraocular pressure assessment in patients with lysosomal storage diseases. J PloS One. 2017;12:e0168698.
- Aiello LM. Perspectives on diabetic retinopathy. Am J Ophthalmol. 2003;136:122-135.
- Day AC, Dhariwal M, Keith MS, Ender F, Vives CP, et al. Distribution of preoperative and postoperative astigmatism in a large population of patients undergoing cataract surgery in the UK. Br J Ophthalmol. 2019;103:993-1000.
- Ladeveze ER, Ortiz AM, Visciarelli LA, Cavatorta AE. Corneal Astigmatism in cataract surgery candidates. Braz J Ophthalmol. 2018;77:272-277.
- Varoniukaite A, Vaičaite L, Kuzmiene L. Biometric parameters, corneal astigmatism and ocular comorbidity in cataract surgery patients. J Med Sci. 2018;1:1-10.
- Ferreira TB, Hoffer KJ, Ribeiro F, Ribeiro P, O’Neill JG. Ocular biometric measurements in cataract surgery candidates in Portugal. PloS One. 2017;12:e0184837.
- Curragh DS, Hassett P. Prevalence of corneal astigmatism in an NHS cataract surgery practice in Northern Ireland. Ulster Med J. 2017;86:25.
- Shori C, Shori R, Laxmiprasad G. study of clinical and ophthalmologic profile of patients undergoing cataract surgery. Intern J Res Med Sci. 2017;5:2229-2232.
- Chaudhary M, Dahal H. Prevalence and types of corneal astigmatism in patients undergoing cataract surgery. J Inst Med. 2017;41:22-28.
- Prasher P, Sandhu JS. Prevalence of corneal astigmatism before cataract surgery in Indian population. Intern Ophthalmol. 2017;37:683-689.
- Gohari M, Noorizaheh F, Salimpur S, Aghayi M, Besharati MR. Prevalence of corneal astigmatism before cataract surgery in yazd province, Iran. J Ophthal Optomet Sci. 2016;1:14-18.
- Liu Y, Congdon NG, Fan H, Zhao X, Choi K, et al. Ocular comorbidities among cataract-operated patients in rural China: the caring is hip study of cataract outcomes and uptake of services (SCOUTS), report No. 3. Ophthamoloygy. 2007;114:e47-e52.
- Pham TQ, Wang JJ, Rochtchina E, Maloof A, Mitchell P. Systemic and ocular comorbidity of cataract surgical patients in a western Sydney public hospital. Clin Exp Ophthalmol. 2004;32:383-387.



