Research Article - Onkologia i Radioterapia ( 2021) Volume 15, Issue 9
Estimated doses of folinic acid after methotrexate high dose in hematologic malignancies
Zainab Mustafa Mahdi*Zainab Mustafa Mahdi, College of Pharmacy, University of Tikrit, Salahaldeen, Iraq, Email: rawaqjasim@gmail.com
Received: 17-Jul-2021 Accepted: 26-Aug-2021 Published: 31-Aug-2021
Abstract
Folinic acid is a metabolically active reduced form of folate that bypasses dihydrofolate reductase. Folate supplementation indications include the prevention of several diseases such as ulcerative colitis, neural tube defects, and cognitive dysfunction in the elderly. As a derivative of folic acid, folinic acid is useful as an antidote to folic acid antagonists (i.e., methotrexate, pyrimethamine). Folinic acid may be administered to counteract the potential toxicity of methotrexate that escapes into the systemic circulation. A clinical prospective follow up study conducted in Baghdad Hematology center of Medical city during the period from 1st of November, 2018 to 20th of April, 2019on sample of 53 Iraqi patients with hematological malignancy. The diagnosis of acute lymphoblastic leukemia or non-Hodgkin's lymphoma was done by the physicians through proper investigations. The Methotrexate dose and infusion rate were designed by the protocols. The patients were followed through serum collection and estimation of Methotrexate level by Abbut Machine and followed by administered the folinic acid doses based on Methotrexate level. MTX serum level should be measured after 24, 48, and 72 hour after administration. Folinic acid doses should be given according to the level of HDMTX.
Keywords
folinic acid, folate, methotrexate, NHL, ALL
Introduction
Folinic acid (5-formyltetrahydrofolate ([R, S] 5-CHOFH4)) is a naturally occurring, reduced form, of folic acid commonly known in clinical practice as leucovorin. Often, clinicians use the terms folic acid and folinic acid interchangeably, but they are, in fact, not the same. Folic acid is a synthetic, oxidized, and water-soluble form of folate (vitamin B9) that is used therapeutically and does not exist in nature, whereas folinic acid exists naturally and is biologically active [1]. Folinic acid is a metabolically active reduced form of folate that bypasses dihydrofolate reductase [2]. Folate supplementation indications include the prevention of several diseases such as ulcerative colitis, neural tube defects, and cognitive dysfunction in the elderly [1]. As a derivative of folic acid, folinic acid is useful as an antidote to folic acid antagonists (i.e., methotrexate, pyrimethamine) [3]. Leucovorin may be administered to counteract the potential toxicity of methotrexate that escapes into the systemic circulation 4. Frequently referred to as “leucovorin rescue,” folinic acid is used to counteract the toxic effects of high dose methotrexate therapy for more than 30 years, leucovorin rescue has been a cornerstone of HDMTX treatment. Leucovorin is particularly effective in the prevention of myelosuppression, gastrointestinal toxicity, and neurotoxicity during treatment with HDMTX. Chemotherapy protocols that include HDMTX also include recommendations for the timing, dose, and duration of leucovorin administration to protect normal cells from injury [3].
Folates and folic acid are not biologically active and must be converted into tetrahydrofolate by way of dihydrofolate reductase. Folinic acid does not require dihydrofolate reductase for conversion into tetrahydrofolate [1]. Tetrahydrofolate and its derivatives then go on to participate in thymidylate and purine synthesis as they are essential in carrying out one-carbon transfer reactions in vivo [4]. These reactions are especially important in the generation of nucleic acids, the regulation of gene expression, and the overall stability of the genome [5]. Folinic acid is compounded with calcium in the form of leucovorin calcium (especially for FDA approved indications), and can be administered intramuscularly, intravenously, or orally. The timing, dosage, and route of folinic acid administration depend on the desired outcome for the desired indication [6]. Leucovorin is administered at a dose per institutional guidelines before administration of glucarpidase and at a dose of 250 mg/m2 IV every 6 hours for 48 hours after administration of the last dose of glucarpidase. The dose and duration of subsequent leucovorin rescue was based on plasma MTX concentration determined by reverse phase high-performance liquid chromatography or by commercial MTX assay [7].
Methods
Study design and settings
This study is a clinical prospective study conducted in Baghdad Haematology centre of Medical city during the period from 1st of November, 2018 to 20th of April, 2019.
Study population
Patients with haematological malignancy (47 ALL patients and 6 NHL patients) admitted to Baghdad Haematology centre of Medical city for Methotrexate treatment were enrolled in the study.
Sampling
A convenient sample of 53 Iraqi patients with haematological malignancy admitted to Baghdad Haematology centre for MTX treatment according to chemotherapy protocol. Patients were pre-treated with iv fluids (25 patients received 2 L while 28 patients received 3L) either NS or GS with sodium bicarbonate for alkalization 45cc and potassium chloride 15cc-30cc started 12 hr before administration of MTX. After the patients who received MTX either over 24 hr. infusion (48 patients) or over 4 hr. infusion (5 patients) the dose of 15 mg/m2 every 6 hr folinic acid was administered 12 hr after finishing MTX infusion, then blood samples drown by nurses after 24,48,72 hr and then measured MTX serum level by Abbut machine.
Results
This study included 53 Iraqi patients with hematological malignancy presented to Baghdad Hematology center of Medical City. Mean age of patients with hematological malignancy was 26.7 ± 11.8 years; 43.4% of patients were in age group 14 years and more, 18.9% of them were in age group 20-29 years, 15.1% of them were in age group 30-39 years and 22.6% of them were in age 40-49 years. Male patients with hematological malignancy were more than female patients with male to female ratio as 1.6:1. All these findings were shown in table 1 and figure 1.
| Variable | No. of patients | % |
|---|---|---|
| Age mean ± SD (26.7 ± 11.8 years) | ||
| ≥ 14 years | 23 | 43.4 |
| 20-29 years | 10 | 18.9 |
| 30-39 years | 8 | 15.1 |
| 40-49 years | 12 | 22.6 |
| Total | 53 | 100 |
| Gender | ||
| Female | 20 | 37.7 |
| Male | 33 | 62.3 |
| Total | 53 | 100 |
Tab. 1. Demographic characteristics of patients with hematological malignancy
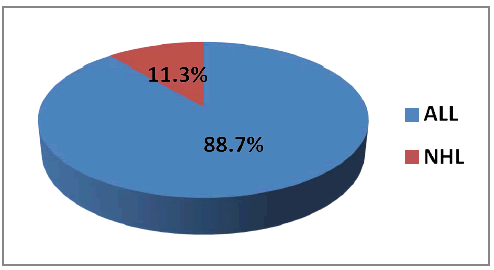
Figure 1: Diagnosis of haematological malignancy
The common diagnosis of patients with haematological malignancy was Acute Lymphocytic Leukemia (ALL) (88.7%); followed by Non-Hodgkin's Lymphoma (11.3%). All these findings were shown in figure 1.
Mean Methotrexate (MTX) dose for patients with hematological malignancy was 2904.4 ± 1463.1 mg and mean body surface area of them as 1.85 ± 1.41 cm2 with mean dose/BSA as 1756.1 ± 950.9 mg/cm2. Mean serum level of MTX 24 hr was 0.53 ± 0.67 mg, for 48 hr was 0.37 ± 0.49 mg and for 72 hr was 0.47 ± 0.86 mg. All these findings were shown in tables 2 and 3.
| Variable |
|---|
| Total dose of MTX (2904.4 ± 1463.1 mg) |
| BSA (1.85 ± 1.41 cm2) |
| Dose/BSA (1756.1 ± 950.9 mg/cm2) |
| Serum level of MTX 24 hrs (0.53 ± 0.67 mg) |
| Serum level of MTX 48 hrs (0.37 ± 0.49 mg) |
| Serum level of MTX 72 hrs (0.47 ± 0.86 mg) |
Tab. 2. Methotrexate dose and serum levels of patients with hematological malignancy
Most (98.1%) of patients with hematological malignancy were treated with 15 mg folinic acid and only one patient was treated with 300 mg folinic acid. Number of folinic acid doses was 4 doses for 50.9% of patients with hematological malignancy, 8 doses for 37.8% of them and 12 doses for 11.3% of them. All these findings were shown in table 3.
| Variable | No. of patients | % |
|---|---|---|
| Folinic acid dose mean ± SD (20.4 ± 39.1 mg) | ||
| 15 mg | 52 | 98.1 |
| 300 mg | 1 | 1.9 |
| Total | 53 | 100 |
| Number of folinic acid doses | ||
| 4 doses | 27 | 50.9 |
| 8 doses | 20 | 37.8 |
| 12 doses | 6 | 11.3 |
| Total | 53 | 100 |
Tab. 3. Folinic acid doses of patients with hematological malignancy
No significant differences were observed between hematological malignancy patients with 15 mg folinic acid dose and hematological malignancy patients with 300 mg dose regarding serum MTX 24 hr (p=0.2) and serum MTX 48 hr (p=0.7). All these findings were shown in table 4.
| Variable | 15 mg | 300 mg | p value |
|---|---|---|---|
| Mean ± SD | |||
| Serum MTX 24hr | 0.53 ± 0.67 | 0.29 ± 0.00 | 0.2*NS |
| Serum MTX 48hr | 0.38 ± 0.5 | 0.24 ± 0.00 | 0.7*NS |
| Serum MTX 72hr | 0.46 ± 0.85 | - | |
| *Independent sample t-test, NS=Not Significant. | |||
Tab. 4. Distribution of serum MTX levels according to folinic acid dose
As shown in table 5, no significant differences were observed between hematological malignancy patients on different folinic acid number of doses regarding serum MTX 42 hr (p=0.7), serum MTX 48 hr (p=0.5) and serum MTX 72 hr (p=0.2).
| Variable | 4 doses | 8 doses | 12 doses | p value |
|---|---|---|---|---|
| Mean ± SD | ||||
| Serum MTX 24 hrs | 0.59 ± 0.77 | 0.47 ± 0.53 | 0.41 ± 0.68 | 0.7*NS |
| Serum MTX 48 hrs | 0.24 ± 0.25 | 0.42 ± 0.58 | 0.67 ± 0.87 | 0.5*NS |
| Serum MTX 72 hrs | 0.05 ± 0.03 | 1 ± 1.3 | - | 0.2**NS |
| *One way ANOVA analysis, **Independent sample t-test, NS=Not significant | ||||
Tab. 5. Distribution of serum MTX levels according to protocols
No significant differences were observed between hematological malignancy patients with MTX serum level ≤ 0.2 and hematological malignancy patients with MTX serum level >0.2 regarding serum folinic acid doses (p=0.3) and number of doses (p=0.3), however, folinic dose was increased among patients with MTX level of more than 0.2. All these findings were shown in table 6.
| Variable | ≤ 0.2 | >0.2 | p value |
|---|---|---|---|
| Mean ± SD | |||
| Folinic acid dose | 15 ± 0.0 | 25.9 ± 55.8 | 0.3*NS |
| Number of doses | 6 ± 2.8 | 6.7 ± 2.7 | 0.3*NS |
| *Independent sample t-test, NS=Not Significant | |||
Tab. 6. Distribution of folinic acid levels and doses according to MTX serum level after 24 hrs
Discussion
Folinic acid is the antidote of choice for treating MTX toxicity. This rescue regimen replenishes intracellular stores of reduced folate and attenuates the MTX toxicity. Serum MTX levels should be measured every 24 hrs until the levels fall below 0.2 μmol/L [8]. Plasma methotrexate concentrations should be monitored closely to detect any delay in methotrexate clearance during each cycle of therapy [9]. Depending on the regimen, plasma methotrexate assays may be appropriate at 24 hrs, 48 hrs, and 72 hrs after the start of methotrexate infusion [10].
Current study showed no significant differences between haematological malignancy patients on different folinic acid number of doses regarding serum MTX 42 hr (p=0.7), serum MTX 48 hrs (p=0.5) and serum MTX 72 hrs (p=0.2). This finding is in agreement with the oncologist study of prevention and management toxicity of high dose MTX in which leucovorin doses are adjusted according to plasma methotrexate concentrations, and hydration and alkalization can be fine-tuned to optimize safety [4].
In most Iraqi hospital the hematologist prescribed randomly constant eight doses of folinic acid after each high dose methotrexate because unavailability of the laboratory methotrexate serum level test. The measure methotrexate serum level before administration folinic acid does and administered the folinic acid doses according to MTX serum level instead of random standard number of folinic acid doses have pharmacoeconomic benefit.
Conclusion
MTX serum level should be measured after 24 hrs, 48 hrs, and 72 hrs after administration. Folinic acid doses should be given according to the level of HDMTX.
Conflict of Interest
Authors declare that there is no conflict of interest.
References
- Scaglione F, Panzavolta G. Folate, folic acid and 5-methyltetrahydrofolate are not the same thing. Xenobiotica. 2014;44:480-488.
- Whittle SL, Hughes RA. Folate supplementation and methotrexate treatment in rheumatoid arthritis: a review. Rheumatol. 2004;43:267-271.
- Howard SC, McCormick J, Pui CH, Buddington RK, Harvey RD. Preventing and Managing Toxicities of High-Dose Methotrexate. Oncol. 2016;21:1471-1482.
- Brunton LL, Lazo JS, Parker KL. Goodman & Gilman's: The Pharmacological Basic of Therapeutics. Occup Environ Med. 2006;64:e2.
- Wang S, Wang L, Zhou Z, Deng Q, Li L, et al. Leucovorin Enhances the Anti-cancer Effect of Bortezomib in Colorectal Cancer Cells. Sci Rep. 2017;7:682.
- Greiner PO, Zittoun J, Marquet J, Cheron JM. Pharmacokinetics of (-)-folinic acid after oral and intravenous administration of the racemate. Br J Clin Pharmacol. 1989;28:289-295.
- Widemann BC, Balis FM, Kim A. Glucarpidase, leucovorin, and thymidine for high-dose methotrexate-induced renal dysfunction: Clinical and pharmacologic factors affecting outcome. J Clin Oncol. 2010;28:3979-3986.
- Bhushan M, Singh AL. Acute Methotrexate Toxicity. Indian J Drugs Dermatol. 2015;1:46-49.
- Aumente D, Buelga DS, Lukas JC, Gomez P, Torres A, et al. Population pharmacokinetics of high-dose methotrexate in children with acute lymphoblastic leukaemia. Clin Pharmacokinet. 2006;45:1227-1238.
- Plard C, Bressolle F, Fakhoury M, Zhang D, Yacouben K, et al. A limited sampling strategy to estimate individual pharmacokinetic parameters of methotrexate in children with acute lymphoblastic leukemia. Cancer Chemother Pharmacol. 2007;60:609-620.



