Research Article - Onkologia i Radioterapia ( 2021) Volume 15, Issue 8
Breast cancer in young women of age 35 years and below: Initial experience at a tertiary cancer center in South India
Sithara Aravind1, Geetha Muttath2*, Fathima Bincy2, Mohandoss Murugesan1, Sangeetha K Nayanar1 and Satheesan Balasubramanian32Department of Radiation Oncology, Malabar Cancer Centre, Thalassery, Kerala, India
3Department of Surgical Oncology, Malabar Cancer centre, Thalassery, Kerala, India
Associate Professor. Geetha Muttath, Department of Radiation Oncology, Malabar Cancer Centre, Thalassery, Kerala, India, Email: radpathonc2021@gmail.com
Received: 22-Jul-2021 Accepted: 27-Aug-2021 Published: 17-Sep-2021
Abstract
Introduction: Breast cancer in women aged less than 35 years is uncommon and accounts for 12% of all breast cancer in the West. Breast cancer in young women as defined in our study belongs to 35 years of age and below. In this population, breast carcinoma is the most common malignant disease and has the greatest mortality. Numerous clinical studies have confirmed that breast cancer in young women has a higher histologic grade, unfavourable hormonal status, and overall higher death rate compared to the older population of women. Background of the present study is that clinic pathological and survival data regarding Young Patients with Breast Cancer (YBC) in South Indian population are scarce and heterogeneous. To the best of knowledge there is no study about survival in young breast cancer under taken in Kerala population.
Aims and Objectives: To analyse the clinical, pathological, prognostic factors, treatment modalities and survival status of young females with breast cancer treated at our institution.
Materials and Methods: A retrospective single centre study of all female patients of age 35 yrs. and below with histological diagnosis of carcinoma breast, treated from January 2014 to December 2016.
Results: Of total 1686 breast cancer cases registered at our institution, 65 cases were females of age 35 years and below. Median age was 33 years. Four patients (6.1%) had family history of breast cancer. Left breast was the predominant site of occurrence. Infiltrating Ductal Carcinoma, Grade II was the most common histologic type and grade. 14 patients were Estrogen and Progesterone Receptor (ER PR) positive with Her 2 negativity. 60% patients were Her2 positive, irrespective of ERPR status. Most cases belonged to tumour stage T2. Surgery was the main stay of treatment and was undertaken by 90.8% patients (n-59). 5 year Overall Survival (OS) was 90% ,Median disease free survival was 56 months with 5 year Disease Free Survival (DFS) being 43%.Our cohort was divided into two groups, based on age , so as to compare their DFS. The first group belonged to age 25-30 years (n-11) and second group to age 31-35 years (n-54). There was no significant difference in 3 year DFS between the two groups (80% vs 87%, p value=0.432). The median DFS in patients was 56 (44-67) months, while median DFS was not attained in patients less than 30 years.
Conclusion: According to our study, the incidence of breast cancer in young females is high when compared to the published Western data but lower than available Indian data. It is also found to occur at a much younger age. The unique finding in our study is that though the patients present with Grade 2/3 invasive ductal carcinoma with a higher incidence of HER2 positivity, the 5 Year OS is 90% indicating a good survival status which is in contrast with the Western literature.
Keywords
breast cancer, young women, clinicopathologic features, survival
Introduction
Breast cancer is the most common cancer affecting women globally, accounting for 25.4% of all new cancer cases diagnosed. It is the leading cause of cancer death in 103 countries including India [1]. Breast cancer in women aged less than 35 years is uncommon and accounts for 1%-2% of all breast cancers worldwide [1]. Clinical studies from West show that when compared to the older population, breast cancer in young women has a higher histologic grade, unfavourable hormonal status, and higher death rate [2].
Recent years has noted a trend of increasing incidence of young breast cancer in India [3, 4]. The incidence of breast cancer in young Indian women is seen to be associated with aggressive histology and loss of Estrogen and Progesterone Receptor expression [5-8]. Thorough literature search reveals a paucity of data on survival in young breast cancer patients in India.
Background of the present study is that clinicopathological and survival data regarding Young Patients with Breast Cancer (YBC) in South Indian population are scarce and heterogeneous. To the best of knowledge there is no study about survival in young breast cancer under taken in Kerala population. We aim to analyse the clinical, pathological, prognostic factors, treatment modalities and survival status of young females with breast cancer treated at our institution.
Methodology
A retrospective study was initiated at our centre after approval from Institutional Review Board. All female patients of age 35 years and below with histological diagnosis of carcinoma breast, treated from January 2014 to December 2016 were included in the study. Patients who were lost to follow up and patients whose case records had incomplete data were excluded.
Demographic, clinical, treatment and follow up details were collected from Medical Case records. Histomorphological details and Immuno Histo Chemical (IHC) status (of Estrogen, Progesterone and Her2 receptors) were obtained from histopathology records, and wherever necessary, Haematoxylin and Eosin stained slides and IHC slides were reanalysed by the pathologist. Histopathologiceporting was done as per CAP protocol (College of American Pathologists). Cancer staging done as per TNM classification in American Joint Committee on Cancer Staging System for Breast Cancer-2010. Histologic grading of breast carcinoma was performed using Nottingham Histologic Score. Ki-67 was not routinely done at our centre during the study period.
Patients with Early Breast Cancer (EBC) were treated with Breast Conservation Surgery (BCS)/Modified Radical Mastectomy (MRM), followed by adjuvant treatment, whereas those with Locally Advanced Breast Cancer (LABC) were treated with neoadjuvant chemotherapy followed by surgery and adjuvant treatment. Women with upfront metastatic disease were treated with palliative intent. Chemotherapy with Adriamycin 60 mg/m2 and Cyclophosphamide 600 mg/m2 followed by Taxanes (12 cycles of weekly Paclitaxel 75 mg/m2) or (4 cycles of 3 weekly Paclitaxel 175 mg/m2) was used. Targeted therapy with Trastuzumab was given to all HER2 positive patients. Tamoxifen or Aromatase inhibitors was given to hormone receptor positive patients. Adjuvant Radiotherapy (RT) was given with 3 Dimensional Conformal RT or 2D RT with breath hold technique in selected patients. All patients received 40 Gy in 15 fractions and an additional boost of 10 Gy in 5 fractions to the tumour bed for patients who underwent BCS.
We attempted to classify our cohort into two groups- Early Breast Cancer (EBC) and Locally Advanced Breast Cancer (LABC), based on the stage of disease at the time of presentation as per AJCC 8th edition Early Breast Cancer (EBC) is defined as Breast cancer that has not spread beyond the breast or the axillary lymph nodes. This includes ductal carcinoma in situ and stage I, stage IIA, stage IIB, and stage IIIA breast cancers. Locally Advanced Breast Cancer (LABC) is a term that encompasses breast cancer that is inoperable or is operable only by mastectomy at initial presentation. This includes T3 or T4 tumours and any N2 or N3 disease [9].
We also grouped the young cancer patients into two, based on age group, so as to compare their Disease Free Survival. The first group belonged to age 25-30 years and second group to age 31-35 years.
Statistical Analysis
The continuous variables were expressed in median (range)/ mean (SD). Kaplan Meier method was used to estimate median OS and DFS, while log rank test was used to compare survival between age groups 25-30 years and 31-35 years. SPSS version 20 was used for statistical analysis. p value of <0.05 was considered statistically significant.
Results
During the study period, 1686 breast cancer cases were registered at our institution, of which 65 cases were females of age 35 years and below. The clinical and demographic details are shown in Table 1. A median age of 33 years (range: 25-35 years) was noted. 58.4%, (n-38) of patients had attained menarche after 12 years and 83% (n-54) were multiparous. . Four patients (6.1%) had family history of breast cancer. Body mass index was <25 in 64.6% (data available for 42 patients) of patients.
| Category | Number (n) | Percentage (%) | |
|---|---|---|---|
| Age | Median (Range) | 33 | 25-35 |
| Family h/o breast cancer | Present | 4 | 6.1 |
| Age at menarche | ≤ 12 | 9 | 13.8 |
| (Median-13 yrs) | >12 | 38 | 58.4 |
| Unknown | 18 | 27.7 | |
| Parity | Nulliparous | 10 | 15.3 |
| Parous | 54 | 83 | |
| Unknown | 1 | 1.5 | |
| Breast feeding | Present | 54 | 83 |
| Body mass index | <25 | 42 | 64.6 |
| 25-29 | 15 | 23.7 | |
| 30 and above | 6 | 9.2 | |
| Unknown | 2 | 3 | |
| Blood group (n-49) | A positive | 7 | 14.2 |
| B positive | 19 | 38.8 | |
| AB positive | 1 | 2 | |
| O positive | 15 | 30.6 | |
| Others | 7 | 14.2 |
Tab. 1. Demographic and clinical details of young women with breast cancer treated from January 2014 to December 2016
Diagnostic modalities
FNAC was the main initial modality of diagnosis and was done in 61.5% (n=39) patients. FNAC was reported as malignant in 92%(n=36) and suspicious for malignancy in 8% (n=3). Mammogram was undertaken by 73.8% (n=48) patients.
Histomorhological and IHC features
Left breast was the predominant site of occurrence. Infiltrating Ductal Carcinoma, Grade II was the most common histologic type and grade (Figure 1). In situ component was seen in 35% (n=23) and were predominantly high grade (17%). The histomorphological and IHC details are shown in Tables 2 and 3 respectively.
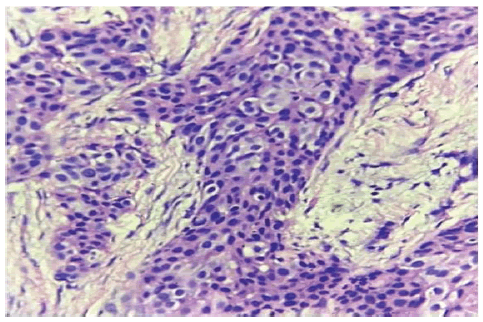
Figure 1: Invasive Ductal carcinoma -H&E,10x
| Number (n) | % | ||
|---|---|---|---|
| Histologic Type | Invasive Ductal Carcinoma | 63 | 97 |
| Invasive Lobular Carcinoma | 2 | 3 | |
| Grade of Tumour | 1 | 1 | 1.5 |
| 2 | 36 | 55.3 | |
| 3 | 22 | 33.8 | |
| Unknown | 6 | 9.2 | |
| Nuclear pleomorphism | Low | 2 | 3.1 |
| Moderate | 47 | 72.3 | |
| High | 4 | 6.2 | |
| Unknown | 12 | 18.4 | |
| Mitosis | <5/hpf | 16 | 24.5 |
| 5-10/hpf | 26 | 40 | |
| >10/hpf | 9 | 13.8 | |
| Unknown | 14 | 21.5 | |
| Carcinoma in situ | Low grade | 2 | 3 |
| Intermediate grade | 10 | 15.3 | |
| High Grade | 11 | 16.9 | |
| Absent | 42 | 64.6 | |
| Lymphovasular Invasion | Present | 11 | 16.9 |
| Perineural Invasion | Present | 4 | 6.1 |
Tab. 2. Histo-pathological parameters young women with breast cancer treated from January 2014 to December 2016
| Hormone status | Number | Percentage |
|---|---|---|
| ER/PR +ve, Her2 –ve | 14 | 21.5 |
| Her2 +ve | 39 | 60 |
| TNBC | 9 | 13.8 |
Tab. 3. IHC details young women with breast cancer treated from January 2014 to December 2016
14 patients were ER (Figure 2) and PR positive with Her2 negativity. 60% patients were Her2 positive (Figure 3), irrespective of ERPR status.
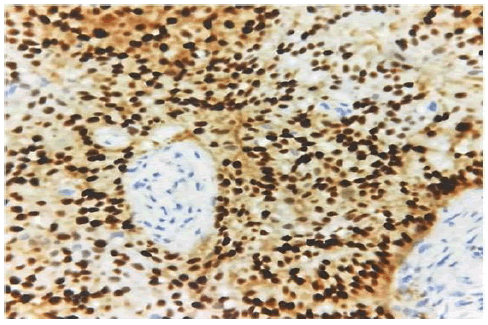
Figure 2: ER positive-IHC-10X
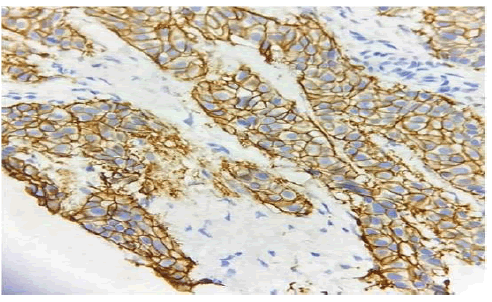
Figure 3: HER2 positive-IHC-10X
Cancer stage and treatment
Most cases belonged to tumour stage T2 (n=33, 50.7%) followed by T3 (n=7, 10.7%). Most of the cases showed absence of nodal metastasis [44.6%, (n=29)]. In node positive cases, N1 stage 15.4% (n=10) predominated. Extra nodal extension was observed in three cases (4.6%). Metastasis was seen only in five (7.7%) cases, the opposite breast being the most common site of metastasis. Surgery was the main stay of treatment and was undertaken by 90.8% patients (n=59). 58.5% (n=38) had undergone Modified Radical Mastectomy, followed by Breast Conservation Surgery in 29.2% (n-19). 27.7% (n=18) received neoadjuvant chemotherapy. Hormone treatment was undertaken by 47.7% (n=31) patients and adjuvant chemotherapy by 87.7% (n=57). 80% (n=52) had received External Beam Radiation Therapy (EBRT), of which 37%(n=24) had received a dose of 40 grey in 15 fractions and 15% (n=10) patients received 50 grey in 25 fractions.
We attempted to classify our cohort into two groups- Early Breast Cancer (EBC) & Locally Advanced Breast Cancer (LABC), based on the stage of disease at the time of presentation (Table 4).
| Variables | EBC n (%) | LABC n (%) |
|---|---|---|
| Number of patients | 44 (67.7) | 21(32.3) |
| HER2 positivity | 27 (61.4) | 12 (57.14) |
| TNBC | 6 (13.9) | 3(14.2) |
| Neo Adjuvant Chemotherapy | 10 (23.8) | 6 (28.6) |
| BCS | 14 (33.3) | 4 (19) |
| MRM | 28 (66.6) | 11(58) |
| Adjuvant Chemotherapy | 41 (93.1) | 21(100) |
| Adjuvant Radiotherapy | 37(88) | 21(100) |
| Tamoxifen | 20 (47.6) | 10 (52.6) |
| EBC: Early Breast Cancer; LABC: Late Breast Cancer | ||
Tab. 4. Comparison of EBC and LABC in young women with breast cancer treated from January 2014 to December 2016
Survival status
5 year Overall Survival (OS) was 90% (Figure 4), Median disease free survival was 56 months with 5 year Disease Free Survival (DFS) being 43% (Figure 5). We attempted to group the young cancer patients into two, based on age group, so as to compare their DFS. The first group belonged to age 25-30 years (n-11) and second group to age 31-35 years (n-54). There was no significant difference in 3 year DFS between the two groups (80% vs 87%, p value=0.432). The median DFS in patients between was 56 (44-67) months, while median DFS was not attained in patients less than 30 years (Figure 6).
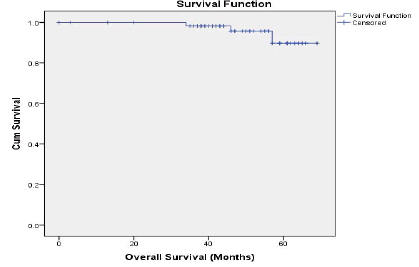
Figure 4: Overall Survival of young women with breast cancer treated from January 2014 to December 2016
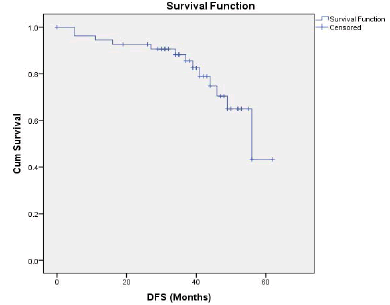
Figure 5: Disease Free Survival of young women with breast cancer treated from January 2014 to December 2016
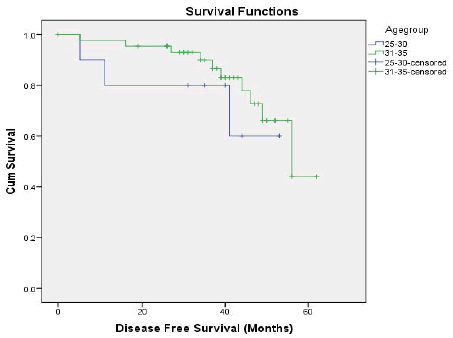
Figure 6: Comparison of DFS of young women with breast cancer treated from January 2014 to December 2016
Discussion
Breast cancer in females of age 35 years and younger, is a rare entity that accounts for 2% of all breast cancer cases in the Western population [10]. Breast cancer in young female patients is increasingly common and presents a serious concern in diagnosis and adequate management of the disease in developing countries [11].
Studies by Mohenthi, et al. and Raina, et al. had shown that the incidence of breast cancer in young women less than 35 years is high in Indian population, accounting to 5.5% and 8% of breast cancer cases respectively [12,13]. Present study showed an incidence of 3.86%, a value less than the above mentioned Indian Studies.
According to the SEER study, the mean age of diagnosis, was 34.8 years while in our study it was 33 years. 10 Studies have shown a decrease in median age of menarche for young breast cancers especially in Spanish population but in our cohort it was 13 years [14].
Nulliparity and usage of Oral Contraceptive pill have shown an inverse association with young breast cancer [15]. We observed that 83% of our study population was multiparous, and none of the patients gave a history of current or past oral contraceptive use both findings in accordance with previous studies.
Obesity is an established risk factor for breast cancer, but in most studies involving premenopausal women an inverse relationship has been found between weight or Body Mass Index (BMI) and breast cancer. The increased incidence of breast cancer in lean young women is found to be strongest amongst the youngest age group (<35 years) [16]. In our study such as an association was not seen- median BMI of patients was 23.3, which means the young women belonged to normal/healthy weight range.
Blood group A with positive Rh subgroup predominated in patients with breast cancer when compared to non-O blood groups [17]. Patients with blood group O were more likely to have favourable prognosis when younger than 40 years [18]. In our study the predominant blood group was B positive.
A positive breast feeding status was given by 84% cases in our study. This observation is in contrast with a study in United Kingdom which shows that that breast feeding protects young women from developing breast cancer [19].
Left breast was the predominant site of occurrence 50.8%, in concordance with previous studies [20]. Histologically, the predominance of infiltrating ductal carcinoma case reported in our study is corroborated in numerous reports in the literature databases [21,22].
Women younger than 35 have a lower rate of ductal carcinoma in situ, but in our study, an interesting observation was that in situ component was seen in 64.6% [23].
Grade 3 was the most common histologic grade (Modified BR) in the Korean study18, while it was Grade 2 in a study conducted in France and in them Lymphovascular emboli was seen in 50.6% of young breast cancer [24]. In our study Grade 2 was most common histologic grade and LVE was seen in 17% of patients.
T2 N0M0 ( Stage IIA) was the most common disease stage in our study population, while in western studies the young women are more likely to be diagnosed at a more advanced stage [25]. We had 41.5% cases with ER PR positivity and 35.4 % cases with HER2 positivity. Hormone positivity of our study population is comparable with French cohort (41.5% vs 39.8%) but with a higher HER2 positivity (35.4% vs 22%).
A 13% 10-year cumulative incidence of contralateral breast cancer has been observed in women under age 36 treated for early-stage breast cancer [26]. We could see a similar observation in our study, in which 75% of those with metastasis had opposite breast as metastatic site. Studies from Mexico have shown a prevalence of LABC that ranges from 43.5% to 68% in young women [27]. Interestingly in our study prevalence of LABC is quite low 32.3%.
Most of the literature shows that across all histologic subtypes and stages, breast cancer survival rates are comparatively lower for women <40 years of age than for older women [28]. But in our study the 5 year OS was 90% indicating a good survival status.
For females diagnosed during 2000-2005,the lowest overall rate of cancer survival, was in those aged 25-29 years (72% 5-year relative survival), followed by 20-24 years old and 30-34 years old (75% and 76%, respectively) and 35 to 39 year old (80%) In contrast, relative survival for women between age 45 and 80 years was 84%-86% [29].Our study shows a similar picture though statistically not significant 25-30 years old group had 3 years DFS of 80% only, when compared to 31-35 years old group with a 3 years DFS of 87%. The shortcomings of the present study were the short study duration and small sample size.
Conclusion
According to our study, the incidence of breast cancer in young females is found to be high when compared to the published Western data. It is also found to occur at a much younger age. Hormone positivity of our study population is comparable with French cohort but with a higher HER2 positivity. The unique finding in our study is that though the patients present with Grade 2/3 invasive ductal carcinoma with a higher incidence of HER2 positivity, the 5 Year OS was 90% indicating a good survival status which is in contrast with the Western literature. This warrants a multicentre study on young breast cancer in Indian population covering the genomic variations of our population aimed at developing prognostic markers and targeted therapy protocols. This should be done hand in hand with steps to increase awareness among young females regarding symptoms, self-examination techniques, the need for early detection and appropriate management.
Conflict of Interest
The authors hereby agree that the manuscript has been read and approved by all the authors, that the requirements for authorship as stated earlier in this document have been met, and that each author believes that the manuscript represents honest work.
References
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209-249.
- Martínez MT, Oltra SS, Pena-Chilet M, Alonso E, Hernando C, et al. Breast cancer in very young patients in a spanish cohort: age as an independent bad prognostic indicator. Breast Cancer: Basic Clin Res. 2019;13:1-10.
- Varughese AA, Poothiode U, and Manjula VD. Descriptive study on selected risk factors and histopathology of breast carcinoma in a tertiary care centre in Kerala, India with special reference to women under 40 years old. Asian Pac J Cancer Prev. 2015;16:181-184.
- Gogia A, Raina V, Deo SV, Shukla NK, and Mohanti BK. Young breast cancer: A single center experience. Indian J Cancer. 2014;51:604-608.
- Takalkar UV, Asegaonkar SB, Kulkarni U, Kodlikeri PR, Kulkarni U, et al. Clinicopathological profile of breast cancer patients at a tertiary care hospital in marathwada region of Westen India. Asian Pac. J. Cancer Prev. 2016;17:2195-2198.
- Parmar V. Rising Incidence of Breast Cancer in the Young Fertile Indian Population-a Reality Check. Indian J Surg Oncol. 2018;9:296-299.
- Deshmukh SP, Mane AD, Zade BP, and Sane SP. Breast cancer in young women in India. Ann Oncol. 2012;23:101.
- Ghosh S, Sarkar S, Simhareddy S, Kotne S, Rao PB, et al. Clinico-morphological profile and receptor status in breast cancer patients in a South Indian institution. Asian Pac J Cancer Prev. 2014;15:7839-7842.
- Edition S, Edge SB, and Byrd DR. AJCC cancer staging manual. Ca Cancer J Clin. 2017.
- Howlader NN, Krapcho M, Miller D, Bishop K, Kosary CL, et al. SEER Cancer Statistics Review (CSR) 1975-2014. Cancer Stat Rev. 2020: 1975-2017.
- Coebergh JW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374-1403
- Mohanti BK, Raina V, Gogia A, Deo SVS, Shukla NK. Young patients with breast cancer (<35 years): Single-institution study of 194 patients from India. J Clin Oncol. 2012;e11013.
- Raina V, Gogia A, Mohanti BK, Deo SVS, Shukla NK. Breast cancer in the young (=35 years): A single center study from the All India Institute of Medical Sciences. J Clin Oncol. 2013; e12539
- Pollan M, Pastor-Barriuso R, Ardanaz E, Arguelles M, Martos C, et al. Recent changes in breast cancer incidence in Spain, 1980-2004. J Natl Cancer Inst. 2009;101:1584-1591
- Anderson WF, Matsuno RK, Sherman ME, Lissowska J, Gail MH, et al. Estimating age-specific breast cancer risks: a descriptive tool to identify age interactions. Cancer Causes Control. 2007;18:439-447
- Carmichael AR, Bates T. Obesity and breast cancer: a review of the literature. Breast. 2004;13:85-92.
- Holdsworth PJ, Thorogood J, Benson EA, Clayden AD. Blood group as a prognostic indicator in breast cancer. Br Med J (Clin Res Ed). 1985;290:671-673.
- Park S, Kim KS, Kim JS. Prognostic value of ABO blood types in young patients with breast cancer; a nationwide study in Korean Breast Cancer Society. Med Oncol. 2017;34:118.
- Breast feeding and risk of breast cancer in young women. United Kingdom National Case-Control Study Group. BMJ. 1993;307:17-20
- Darré T, Tchaou M, Folligan K, Amadou A, N'Timon B, et al. Breast cancer cases of female patients under 35 years of age in Togo: A series of 158 cases. Mol Clin Oncol. 2017;7:1125-1129.
- Greenlee RT, Murray T, Bolden S, Wingo PA. Cancer statistics. CA Cancer J Clin. 2000;50:7-33
- Gueye M, Kane Gueye SM, NdiayeGueye MD, NiasseDia F, Gassama O, et al. Breast cancer in women younger than 35 years: Features and outcomes in the breast unit at aristideledantec teaching hospital, dakar. Med Sante Trop 2016;26:377-381
- Winchester DP, Osteen RT, Menck HR. The national cancer data base report on breast carcinoma characteristics and outcome in relation to age. Cancer. 1996;78:1838-1843
- Erić I, PetekErić A, Kristek J, Koprivčić I, Babić M. Breast cancer in young women: Pathologic and immunohistochemical features. ActaClin Croat. 2018;57:497-502.
- Nixon AJ, Neuberg D, Hayes DF, Gelman R, Connolly JL, et al. Relationship of patient age to pathologic features of the tumor and prognosis for patients with stage I or II breast cancer. J ClinOncol 1994;12:888-894.
- Lee KD, Chen SC, Chan CH, Lu CH, Chen CC, et al. Increased risk for second primary malignancies in women with breast cancer diagnosed at young age: A population-based study in Taiwan. Cancer Epidemiol Biomarkers Prev. 2008;17:2647-2655
- Villarreal-Garza C, Lopez-Martinez EA, Muñoz-Lozano JF, Unger-Saldaña K. Locally advanced breast cancer in young women in Latin America. E cancer medical science. 2019;22:894
- Bleyer A, O'Leary M, Barr R, Ries L, Bethesda MD. Cancer epidemiology in older adolescents and young adults 15 to 29 years of age, including SEER incidence and survival: 1975-2000. National Cancer Inst. 2006.
- Anders CK, Johnson R, Litton J, Phillips M, Bleyer A. Breast cancer before age 40 years. Semin On col. 2009;36:237-249



