Research Article - Onkologia i Radioterapia ( 2025) Volume 19, Issue 5
AI-driven radiotherapy appointment optimization: A lean management approach
Samia Khalfi1,2,3*, T. Malih4, EL M. Abiza2, EL M. Sadiki2, N Chenfour4, Y. Aghlallou3, W. Hassani1,2,3, FZ Farhane1,2,3, Z. Alami1,2,3 and T. Bouhafa1,2,32Department of Radiotherapy, Hassan II University Hospital, Fez, Avenue Hassan II, Fez 30050, Morocco
3Cancer Research Institute (IRC), 224Q+8V, Fes, Morocco
4School of Engineering and Applied Sciences, Morocco
Samia Khalfi, Department of Medicine and Pharmacy of Fez, Boite Postale 1893 - KM 2.200 Route Sidi Harazem Fès, 30070, Morocco, Email: samia.khalfi@gmail.com
Received: 24-Mar-2025, Manuscript No. OAR-25-163085; , Pre QC No. P-163085; Editor assigned: 26-Mar-2025, Pre QC No. P-163085; Reviewed: 09-Apr-2025, QC No. Q-163085; Revised: 16-Apr-2025, Manuscript No. R-163085; Published: 30-Apr-2025
Abstract
Purpose: Radiotherapy is integral to cancer treatment, but inefficiencies in appointment scheduling often lead to delays, suboptimal resource utilization, and compromised care quality. Leveraging Lean Management methodologies, we identified bottlenecks and inefficiencies in the scheduling process, emphasizing the need for advanced optimization strategies. This study developed an AIdriven system to automate and optimize radiotherapy appointment scheduling, integrating patient-specific and departmental constraints.
Materials and Methods: Lean Management tools, including Value Stream Mapping (VSM) and 5S analysis, identified inefficiencies in manual scheduling, such as resource misallocation and delays in urgent cases. An AI-based solution was designed with supervised machine learning algorithms to classify patient urgency and optimize schedules dynamically. The AI system includes data extraction, feature engineering, and real-time optimization modules, ensuring adaptability to workflow variations and emergency cases.
Results: Machine learning models were evaluated for urgency classification, with Random Forest achieving the best performance (AUC: 0.81). The system categorized patients into three priority levels (37.1% Group 1, 35.2% Group 2, 27.6% Group 3) and optimized resource utilization by minimizing scheduling conflicts and delays. The automated process improved workflow consistency, reduced physician workload, and ensured timely treatment for high-priority patients.
Conclusion: AI-driven optimization, combined with Lean Management insights, offers a transformative solution to radiotherapy scheduling challenges, improving care efficiency and resource management in high-demand clinical settings.
Keywords
Artificial intelligence; Radiotherapy; Machine learning; Patient prioritization;Lean managment
Introduction
Radiotherapy is a cornerstone in cancer treatment, and the efficiency of care largely depends on the meticulous planning of patient appointments. Due to the complexity of treatments, which require precise synchronization of resources (medical staff, equipment, and treatment room availability), inefficiencies in scheduling can lead to delays, increased waiting times, and service overload. These dysfunctions directly impact the quality of care and patient satisfaction while increasing pressure on medical teams. In response to these challenges, lean management, a methodology initially developed in the industrial sector to optimize processes and reduce waste, was introduced into our radiotherapy department. This approach allowed us to conduct an in-depth analysis of internal processes and identify major weaknesses in patient flow management, particularly in appointment scheduling [1,2].
Through this methodology, we mapped the entire process—from patient admission to the scheduling of treatment sessions—and identified bottlenecks, redundancies, and areas of variability. By actively involving the department’s staff in this approach, we uncovered several inefficiencies in appointment management, such as unused slots, scheduling conflicts, and extended delays that could postpone treatments or disrupt the workflow of the medical teams. The analysis derived from lean management highlighted improvement opportunities that could not be easily addressed with traditional management methods. In this context, the need for a more flexible and responsive solution, such as Artificial Intelligence (AI), emerged as a suitable response to the growing demands for planning and workflow optimization in radiotherapy. AI, with its ability to analyze large amounts of data and optimize complex processes in real-time, proved to be a promising solution [3].
The objective of our study was to develop an AI system capable of automating and optimizing radiotherapy appointment scheduling by integrating the specific constraints of both the patients and the department, while adapting to unforeseen circumstances and variations in workflow.
MATERIALS AND METHODS
Initial analysis with lean management
The initial analysis of the radiotherapy scheduling system using lean management revealed a chaotic process in the manual scheduling of treatment start dates. This process, primarily handled by the physicians themselves, lacked structure and standardization, often resulting in delays, even for patients requiring urgent treatment. To objectively identify these dysfunctions, several lean management tools were employed. The first tool used was Value Stream Mapping (VSM), which enabled us to map the entire workflow from the initial treatment request to the first radiotherapy session. This mapping revealed significant inconsistencies, with uncoordinated steps in scheduling, resource allocation, and treatment validation, leading to poor prioritization of patients based on the urgency of their cases.
Another key tool was the 5S analysis, which helped structure and organize scheduling tasks by identifying waste. This method highlighted that many treatment slots were either wasted or poorly allocated, increasing pressure on available resources. Moreover, scheduling was performed directly by physicians, a task that consumed a significant amount of their time at the expense of their clinical responsibilities. One of the main effects of this disorganized planning was the accumulation of delays in treatment initiation, particularly affecting patients requiring urgent care. Due to poor priority management, some patients waited several days or even weeks before beginning radiotherapy.
Additionally, the absence of a centralized and optimized management system led to suboptimal resource utilization. Some slots were left vacant while others were overloaded, creating an imbalanced distribution of workload and equipment usage. Coordination among different stakeholders in the department, particularly physicians and radiology technicians, was challenging to manage manually, increasing the risk of errors and delays. This analysis demonstrated the necessity of a complete overhaul of the scheduling process, including automation and optimization through artificial intelligence tools.
AI selection
Given the inefficiencies revealed by the lean management analysis, it quickly became evident that manual appointment scheduling could no longer meet the growing demands of the radiotherapy department. The accumulated delays, resource overload, and lack of responsiveness to unexpected events required a solution capable of processing large amounts of data in real-time while providing flexibility and precision. Artificial Intelligence (AI) emerged as a logical and promising option to address these challenges.
AI offers several advantages:
- Predictive capability: Machine learning algorithms can analyze historical data to anticipate slot demands, taking into account emergencies, treatment durations, and resource availability.
- Resource optimization: AI can simultaneously manage multiple constraints, including equipment availability, treatment room scheduling, and staff availability, to minimize waiting times and optimize resource usage.
- Flexibility and adaptability: Unlike rigid manual systems, AI can adjust schedules in real-time in case of cancellations, changes in treatment duration, or the addition of urgent patients.
AI solution design methodology
The design of the AI solution followed a workflow optimization approach tailored to the specific constraints of radiotherapy. The first step involved identifying operational needs, such as emergency management, dynamic schedule adjustments, and the optimization of human and material resources. Next, a modular architecture was developed, incorporating a data management system capable of processing information from multiple sources, including patient medical records, equipment availability, and medical staff schedules. Using this data, a predictive module was developed with supervised machine learning algorithms trained on historical data to anticipate future workloads and resource needs. Finally, an optimization module was designed to adjust schedules in real-time, considering patient-specific constraints such as treatment duration and urgency. This module relies on combinatorial optimization techniques to determine the best possible configuration, maximizing efficiency while reducing treatment delays. The entire architecture is coupled with an intuitive user interface, enabling medical and administrative staff to interact with the system seamlessly and efficiently [4,5].
RESULTS
We present the results related to the design and development of our solution, aimed at classifying the urgency level of patients based on medical and demographic parameters to automate their scheduling for treatment initiation. This solution relies on several interconnected modules, each playing a critical role in the processes of data Extraction, Transformation, and Loading (ETL), as well as Exploratory Data Analysis (EDA), feature engineering, and machine learning model training.
Main solution modules
- Database module: Manages connections to the database.
- DataEtl module: Handles data extraction, transformation, and loading from external sources.
- Data_atv module : Provides tools for exploratory data analysis and the creation of new features to improve model accuracy.
- Machine_learning module : Contains methods for training and evaluating machine learning models used for urgency classification.
ETL process
The DataEtl class implements the ETL steps, including data extraction from Excel files, followed by transformation through the removal of outliers and missing values using pandas methods like drop_duplicates() and dropna(). The cleaned data is then loaded into a database as a DataFrame for further analysis.
Exploratory Data Analysis (EDA)
EDA, performed via the Data_atv class, explored correlations between variables using pandas and seaborn libraries. The resulting correlation matrix showed that the analyzed numerical variables were not strongly correlated, suggesting the need to create new variable combinations to enhance model performance Fig. 1.
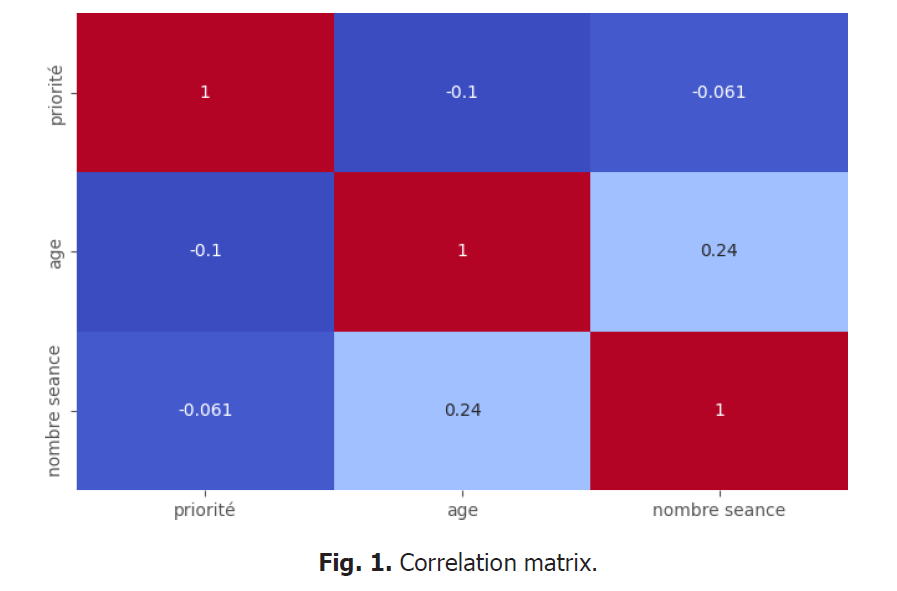
Figure 1: Correlation matrix.
Emergency classification
We established three priority levels to classify patient urgency, ranging from Group 1 (most urgent) to Group 3 (least urgent). The distribution of patients among these groups is relatively balanced, with 37.1% in Group 1, 35.2% in Group 2, and 27.6% in Group 3. This classification enables a more equitable allocation of resources based on medical priorities Fig. 2.
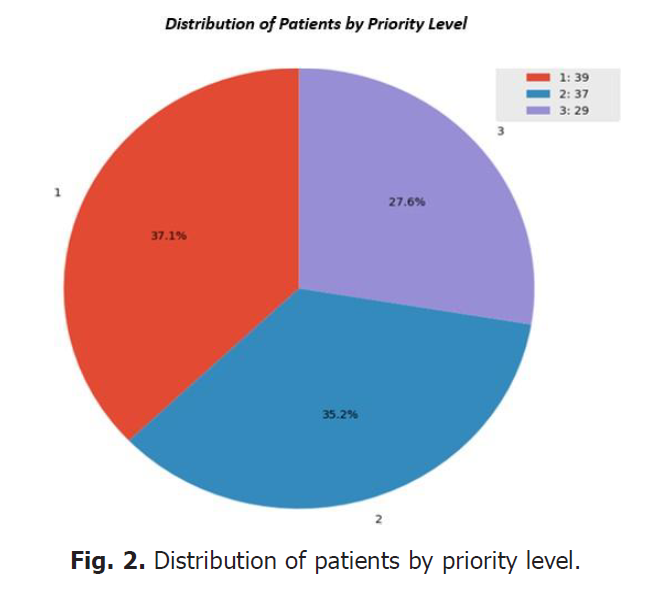
Figure 2: Distribution of patients by priority level.
Distribution of variables
The analysis of the distribution of numerical variables reveals disparities, particularly regarding priority and the number of sessions, which are not centered, while age shows an outlier in the lower part of the distribution. To improve performance, we propose creating binary variables or data combinations to better correlate these variables with the expected outcomes Fig. 3. and Fig. 4.
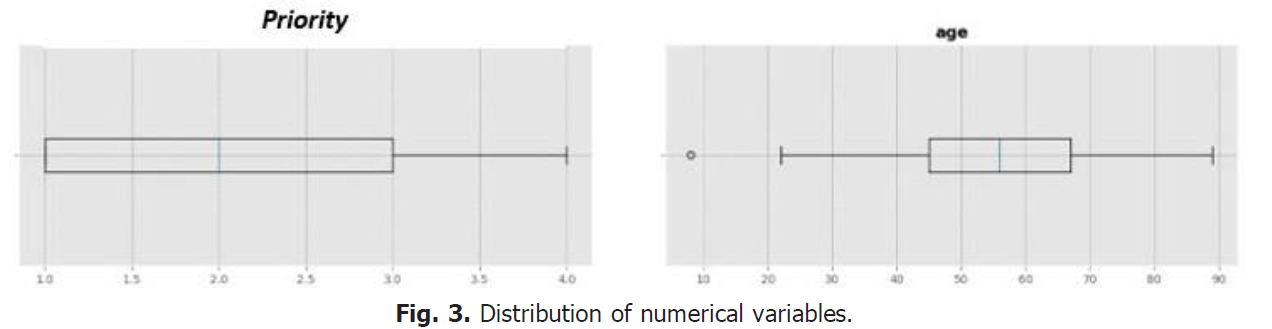
Figure 3: Distribution of numerical variables.
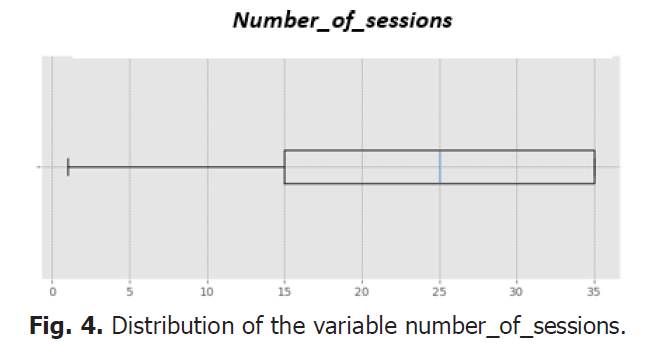
Figure 4: Distribution of the variable number_of_sessions.
Implementation and evaluation of machine learning models
To classify the urgency level of patients, we selected five machine learning algorithms:
- Random forest: A decision tree ensemble that improves accuracy by combining predictions.
- Linear regression: A simple linear model that seeks to establish relationships between the target variable and the explanatory variables.
- Decision tree regressor: A tree-based model that splits the data into homogeneous subgroups.
- KNeighbors regressor: A model based on the proximity of data points, predicting based on the k nearest neighbors.
- MLP Regressor (Multi-Layer Perceptron): A multi-layer neural network capable of capturing non-linear relationships in the data.
Histogram of residuals
The histogram shows the distribution of prediction errors (residuals) for each model. The results indicate that the errors are mainly centered around zero, suggesting that the models make relatively accurate predictions.
ROC curve (Receiver Operating Characteristic):
This curve evaluates the models' ability to discriminate between different classes. The Random Forest model performs the best with an Area Under the Curve (AUC) of 0.81, followed by KNeighbors (0.80), MLP Regressor (0.75), Decision Tree (0.68), and Linear Regression (0.38) Fig. 5 and Fig. 6.
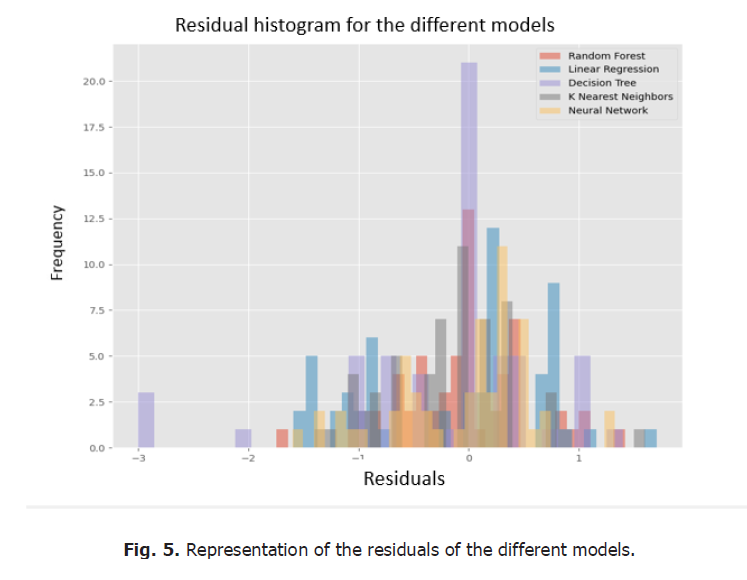
Figure 5: Representation of the residuals of the different models.
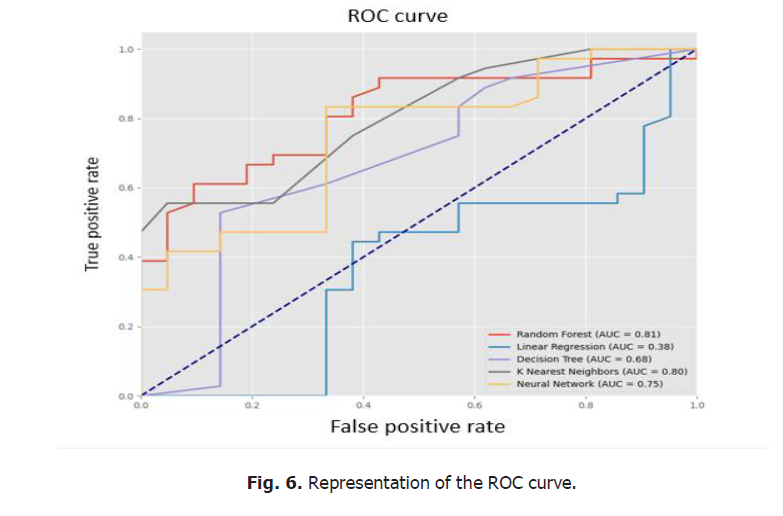
Figure 6: Representation of the ROC curve.
DISCUSSION
The integration of an Artificial Intelligence (AI)-based solution for managing appointments in radiotherapy, specifically for planning the initiation of patient treatments, represents a promising advancement. This approach addresses a critical issue observed during the initial analysis conducted with Lean Management methodology: manual planning was not only inefficient but also a source of Delays for patients requiring urgent care, in addition to monopolizing the doctors' time for administrative tasks. The proposed AI solution was designed to automate this process using medical and demographic criteria, thereby improving resource management and optimizing treatment timelines [4-7].
Interpretation of results
The results from the implementation of the various machine learning models showed that some algorithms, such as Random Forest and KNeighbors Regressor, offered better predictive capacity for determining the degree of urgency of patients, with ROC curves indicating a good ability to discriminate between priority levels. The Random Forest model demonstrated particular robustness in capturing complex, non-linear relationships in the data, which is crucial for classifying patients based on heterogeneous criteria. The low score of Linear Regression highlights the importance of using more flexible models capable of accounting for the complexity of medical data, which cannot be adequately modeled by purely linear relationships. The neural network regression (MLP Regressor), while more effective than linear regression, did not outperform the other models in terms of accuracy, likely due to the limited size of the dataset and the complexity of its optimization.
Practical implications
The application of an AI solution in planning treatment initiation in radiotherapy could have significant implications for resource management and the quality of care provided. Automating this process not only frees up time for doctors, allowing them to focus on higher-value tasks, but also improves the care of more urgent patients. Furthermore, automation ensures consistency in planning by reducing human error and providing better prioritization of patients [7,8].
The results suggest that a more precise classification of urgencies could be achieved by refining the input data. The exploratory study revealed the need to create new features and variable combinations to improve the correlation between demographic and medical factors and the urgency of cases. This could involve, for example, adding binary variables or indicators derived from existing variables to better structure the information.
Limitations and areas for improvement
One of the main limitations of this study is the size and diversity of the dataset used for model training. A larger dataset that includes information from multiple radiotherapy centers could strengthen the robustness of the models and improve their generalization ability. Moreover, although the AI solution was designed to be scalable and adaptable, it has not yet been tested under real-world conditions. Validation in the field is necessary to assess its effectiveness in a clinical environment and to identify required adjustments [9-12].
Another area for improvement would be to integrate additional contextual factors, such as the evolution of patients' medical conditions over time or logistical constraints (machine availability, medical staff leave, etc.), to make the solution even more flexible and tailored to the specific needs of the radiotherapy department [13].
CONCLUSION
The use of artificial intelligence for treatment planning in radiotherapy is an innovative approach that offers potential gains in terms of efficiency, patient prioritization, and reduced treatment delays. The results from this study demonstrate the viability of this approach, although adjustments are still necessary before large-scale implementation. The next steps will involve testing this solution in a real clinical setting and refining the models to further improve classification accuracy and adaptability to departmental needs.
ETHICS
All authors declare that the study was conducted in accordance with the ethical principles of the Declaration of Helsinki. The patients who participated in this study provided written informed consent.
FUNDING
This research is funded by cancer research institute of Morocco (IRC), www.irc.ma» (project n° 1317/AmP 2023).
CONFLICT OF INTEREST
The authors declare no conflicts of interest related to this study.
AUTHOR CONTRIBUTIONS
The role of each author in the design and writing of this article is as follows:
S.K and T.M.; Methodology, S.K and T.M.; Software,S.K and T.M; Validation, S.K and T.M.; Formal Analysis, S.K and T.M.; Investigation, S.K and T.M, E M .A.,N.C,Y.A,W.H,FZ.F, Z.A and T.B.; Resources, all authors; Data Curation; Writing—Original Draft Preparation, S.K, Writing—Review and Editing, S.K and T.M, E M .A.,N.C,Y.A, Visualization, S.K and T.M, E M .A.,N.C,Y.A,W.H,FZ.F, Z.A and T.B Supervision, S.K and T.M, E M .A.,N.C,Y.A,W.H,FZ.F, Z.A and T.B. All authors have read and agreed to the published version of the manuscript.
DATA AVAILABILITY STATEMENT
Data available upon request.
REFERENCES
- Womack JP, Jones DT. Lean thinking—banish waste and create wealth in your corporation. J Oper Res Soc. 1997; 48(11):1148.
- Kollberg B, Dahlgaard JJ, Brehmer PO. Measuring lean initiatives in health care services: Issues and findings. Int J Product Perform Manag. 2006; 56(1):7-24.
- Hall A, Tomásio M. The integration of artificial intelligence in healthcare: Opportunities and challenges. J Health Inform. 2020; 12(2), 123-140.
- Jiang F, Jiang Y, Zhi H, Dong Y, Li H, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017; 2(4).
- Ahmad MI, Khan N. Machine learning in radiotherapy: A review of key techniques and developments. J Radiat Oncol Inform. 2021; 9(3), 150-162.
- Younge KC, Wang L, Monzon JG. Integration of machine learning in radiation oncology: Recent advances and future directions. Radiother Oncol. 2018; 129:421-432.
- Siddique S, Chow JC. Artificial intelligence in radiotherapy. Rep Pract Oncol Radiother. 2020; 25(4):656-666.
- Thompson RF, Valdes G, Fuller CD, Carpenter CM, Morin O, et al. Artificial intelligence in radiation oncology: a specialty-wide disruptive transformation? Radiother Oncol. 2018; 129(3):421-426.
- Chen C, Liu Z, Liang Y, Others. Artificial intelligence in radiotherapy: Applications and challenges. Front Oncol. 2019; (9):1193.
- Dehmer J, Flaherty G, Kim E. Implementing lean in a healthcare setting: A comprehensive review of the literature. Health Serv Res Manag Epidemiol. 2018; (5): 2333392818773451.
- Tucker AL, Heisler WS, Adler-Milstein J. Improving hospital efficiency with lean management: Evidence from multiple case studies. BMJ Quality & Safety. 2016; 25(12): 1008-1014.
- Bennett ME, Cameron KE, Welch MG. The future of artificial intelligence in healthcare: A review of benefits and challenges. Health Care Manag Rev. 2020; 45(2), 153-161.
- Gooding MJ, Smith J. Artificial intelligence in radiotherapy: From automation to decision-support. Clin Oncol. 2019; 31(11), 743-752.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at



